Shifting payer expectations and ongoing reimbursement pressure are pushing physical and rehab therapy organizations to think differently about growth.
Workers’ compensation is gaining traction as a high-potential revenue stream that, when approached strategically, delivers real clinical and financial impact. But success doesn’t come from simply checking the box on workers’ comp.
Return to work programs that deliver real ROI have two things in common: they’re fully integrated into clinical and billing operations, and they deliver clear, job-specific outcomes.
Workers’ Comp as a Strategic Growth Opportunity
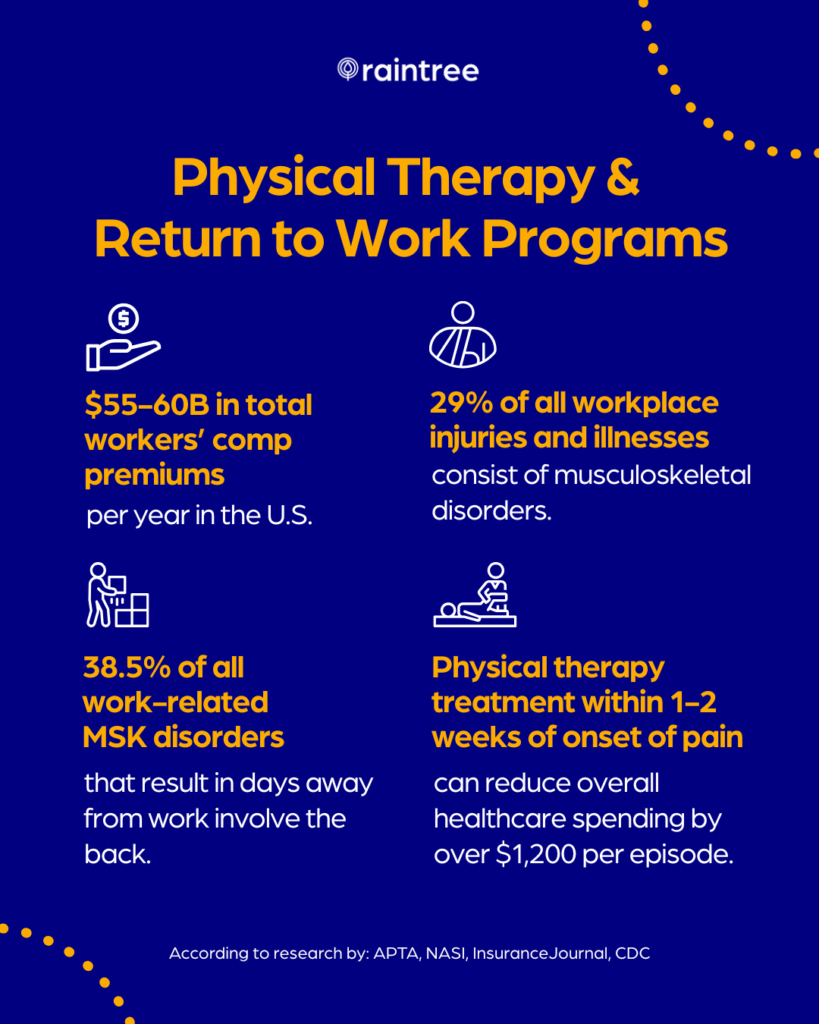
The workers’ comp market is worth an estimated $56 billion, with roughly $4 billion directly tied to physical and occupational therapy services. Yet many rehab organizations still view it as a fringe payer type or operational burden.
That mindset is changing fast. As reimbursement pressure from Medicare and commercial payers intensifies, high-performing therapy groups are turning to workers’ comp programs as a way to diversify revenue and attract steady, high-value referrals.
In fact, for some rehab organizations, workers’ comp accounts for 10–20% of total revenue. As Kathryn Cheng (Raintree’s Head of Partnerships) shared in a recent webinar, “Clinics that lean into this space are unlocking faster reimbursement, stronger referral pipelines, and less administrative burden.”
Better Documentation = Stronger Stakeholder Relationships
A successful return-to-work program doesn’t just serve the patient—it aligns your clinic with the expectations of payers, employers, and other stakeholders like case managers. And this all hinges on documentation that can clearly connects clinical outcomes to job-specific functional goals.
Specialized and complete documentation helps reduce follow-up requests, streamlines approvals, and builds confidence in the quality and value of your practice’s return to work program.
Every payer, every doctor, every case manager gets exactly what they need in one note.
Jim Mecham, MSIE, OTR/L, CPE, Chief Operating Officer & Co-Founder | OccuPro
This level of clarity also drives growth. A structured, outcome-focused RTW program creates a positive feedback loop: better documentation leads to stronger relationships, more referrals, and improved workforce outcomes.
Over time, this can translate into a measurable lift in both revenue and reputation.
Building Your Return to Work Program
For large rehab therapy groups, expanding a return-to-work (RTW) program isn’t just a matter of adding forms or billing codes. Success requires strategic alignment across clinical, operational, and billing workflows.
In this case, the goal is to bypass common operational hurdles (like duplicate documentation, manual claims follow-up, and fragmented communication between departments).
From an operational standpoint, an effective RTW program should help:
- Injured employees return to work faster and more safely.
-
Providers document more efficiently with job-specific functional benchmarks.
-
Billing teams submit clean, compliant claims with fewer rejections.
-
Payers and employers receive timely, actionable updates that support faster decision-making.
Ultimately, high-growth organizations need EMR integrated, cross-functional workflows in order to reduce friction and scale with consistency.
Most issues with claim matching go away when your system helps ensure the data matches what the payer expects.
Alicia Bell, Director of Provider Implementation Services | Jopari
Putting It All Together
When structured around job-specific goals and supported by timely, transparent documentation, a return-to-work program becomes a force multiplier for your revenue cycle.
As the EMR of choice for large and enterprise therapy organizations, Raintree has partnered with leading solutions like OccuPro and Jopari to streamline every stage of the workers’ comp workflow—from initial evaluation and outcomes tracking to claims submission and payment processing.
“There are a lot of systems that say they support workers’ comp,” said Raintree’s Head of Partnerships during Winning the Workers’ Comp Game: Faster Claims, Better Outcomes, and More Revenue. “Supporting isn’t enough anymore—you need a platform that understands it and scales with it.”

