The Centers for Medicare and Medicaid Services (CMS) Calendar Year (CY) 2024 Medicare Physician Fee Schedule Final Rule was published on November 2, 2023.
Spanning a length of over 1,200 pages, the Rule isn’t exactly weekend reading, but it spells out the future of regulatory compliance for clinicians who plan to accept Medicare payments in the next year.
For physical therapy, occupational therapy, and speech-language pathology providers, the upcoming MIPS performance year will bring many important changes. We’ve taken a magnifying glass to the Final Rule, so that you can zoom in on the most important updates for rehabilitation therapists.
2024 Physician Fee Schedule Conversion Factor
Perhaps the most notable change in the 2024 Physician Fee Schedule Final Rule is the reduction of the Medicare Part B conversion factor. The conversion factor for 2024 will be set at $32.74, a reduction of 3.4%.
In previous years, clinicians have successfully advocated for Congress to alleviate the Final Rule conversion factor cut. As a partner to rehabilitation therapy practices, we recommend contacting your representative lawmakers independently or in alignment with professional advocacy organizations.
Performance Policy Changes for Traditional MIPS
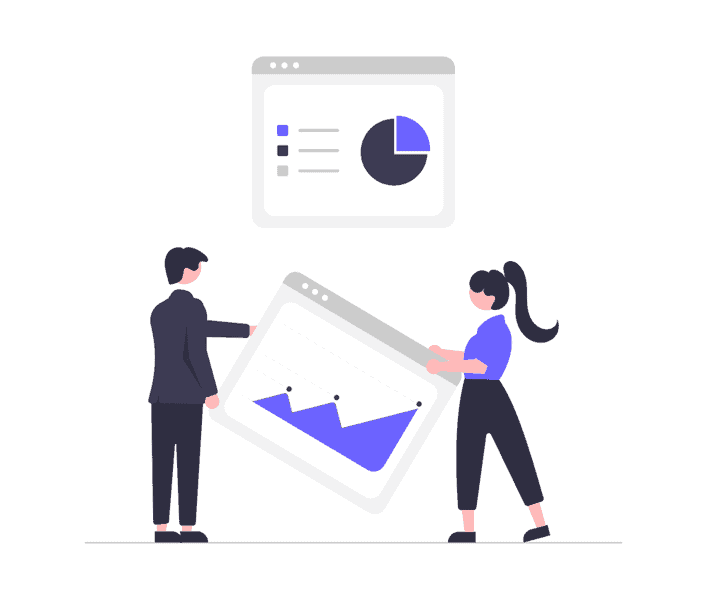
Despite the conversion factor cut, the Final Rule brings some good news. The MIPS Performance Threshold will remain at 75 points for the 2024 reporting period. This is important because your Composite MIPS Score is a key factor in determining payment adjustments for the associated payment year, 2026. Refer to the table below or use the MIPS Payment Adjustment Calculator.
| Composite MIPS Score (2024) | Payment Adjustment (2026) |
|---|---|
| 0 - 18.75 Points | Maximum penalty (-9%) |
| 18.76 - 74.99 Points | Downward payment adjustment (as much as -9%) |
| 75 Points | Neutral adjustment (0%) |
| 75.01 - 100 Points | Positive adjustment (capped at + 9%) |
Data Completeness Requirements
Even though the Performance Threshold will remain at 75 points, providers should take note the 2024 PFS Final rule increases the data completeness threshold to 75% of the eligible instances per measure regardless of payer. This change to the data completeness requirement marks an increase from 70% in 2023.
To meet data completeness criteria for 2024, clinicians must report Quality performance data (“Performance Met,” “Performance Not Met” or denominator exclusions/exceptions) for at least 75% of eligible instances for the entire year, for all collection types.
Development of MVP Reporting for PT and OT
MIPS Value Pathways (MVPs) are a voluntary option for meeting MIPS reporting requirements, as an alternative to traditional MIPS. Each MVP includes a subset of measures and activities related to a specialty or medical condition.
If you’ve followed the direction of regulatory transformation in U.S. healthcare over the last several years, you’ll know that CMS’ goal is to sunset traditional MIPS and transition all clinicians to MVPs.
In keeping with this objective, CMS finalized the introduction of 5 new MVPs for 2024, including the Rehabilitative Support for Musculoskeletal Care MVP, designed for rehabilitation providers like physical and occupational therapists.
Rehabilitative Support for Musculoskeletal Care MVP
In 2024, PTs and OTs will have the option to report using the Rehabilitative Support for Musculoskeletal Care MVP.
The MVP includes 10 quality measures, seven of which use the FOTO measures. The three Musculoskeletal Care MVP Quality measures are:
- BMI Screening
- Falls: Plan of Care
- Screening for Social Drivers of Health.
The episode based Cost measure associated with this MVP is Low Back Pain.
Required Participation for Promoting Interoperability Category
The 2024 Final Rule brought big changes to the Promoting Interoperability Category. Notably, the Promoting Interoperability minimum reporting period increased from 90 to 180 days.
The Final Rule now requires all providers, except social workers, to adopt certified EHR technology (CEHRT) as part of Promoting Interoperability. This change is part of CMS’ goal to move U.S. healthcare into an optimized, digital age where providers collaborate to create better outcomes, using shared patient information. To do so, clinicians need electronic health record systems that can share data securely and seamlessly. The ability of two separate systems to exchange and make use of shared information is called “interoperability.”
Promoting Interoperability and Rehab Therapy
In recent years, occupational therapy, physical therapy, and speech-language pathology providers have been eligible for automatic reweighting of the PI category—meaning that its requirements are unfamiliar to many in our field, including some health IT businesses.
However, as of January 1, 2024, the Promoting Interoperability performance category will no longer be reweighted for OT, PT, and SLP. These provider types must report measures in this category.
Updates to SAFER Guides in 2024
The Final Rule modifies the Safety Assurance Factors for Electronic Health Record Resilience (SAFER) Guides to require MIPS-eligible clinicians to affirmatively attest to completion of the self-assessment of their implementation of safety practices. In 2024, MIPS-eligible clinicians must attest “Yes,” or they will receive a zero for this category.
Exclusions from Promoting Interoperability
Note that practices with 15 or fewer clinicians are not required to submit data for the Promoting Interoperability Category. They are automatically excluded.
Changes to the Cost Performance Category
CMS added 5 new episode-based cost measures to the Cost category, including Low Back Pain (Chronic Pain). This category assesses the treatment and management of low back pain and was designed to capture the range of clinicians that have a role in managing the condition.
Cost scoring has been changed from a measure-level to a category-level. The cost improvement score, which is calculated by CMS, will be calculated over a 2 year period. Therefore, PTs and OTs will not be scored on the Low Back Pain Cost Category until 2024.
How Does CMS Score the Cost Category?
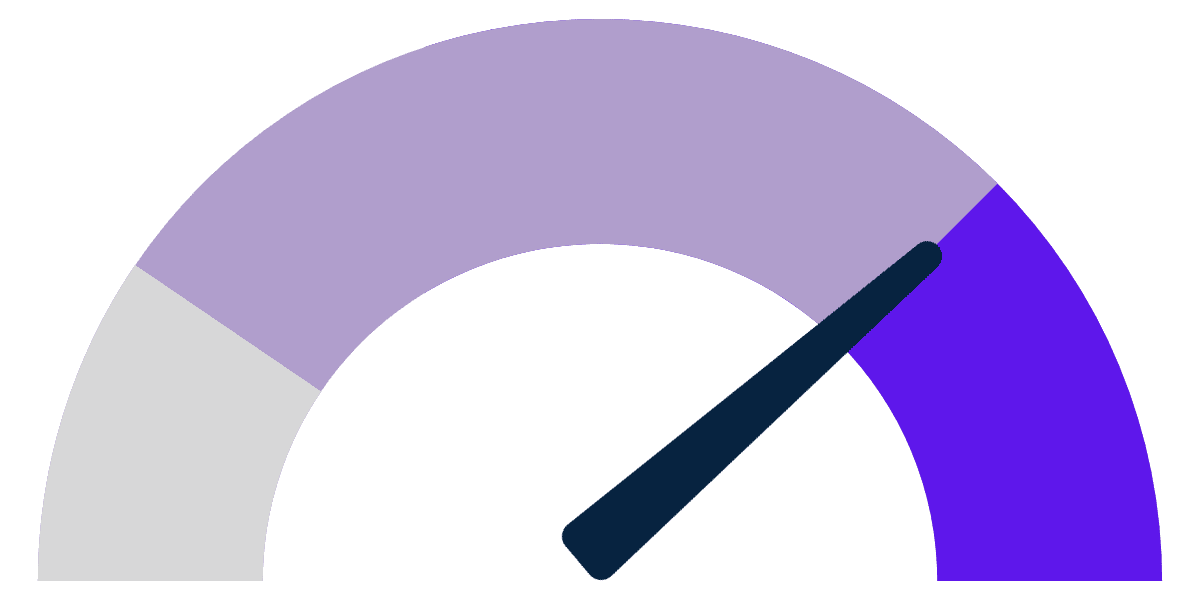
The Cost category was recently re-introduced in 2022, and it represents 30% of the total Composite MIPS Score. For a Cost measure to be scored, the individual or group must exceed the case minimums for the measure. The Cost category relies on claims data; therefore, clinicians do not need to submit anything to participate in this category. The Low Back Cost Category, for example, includes common HCPCS codes used by PT and OT to treat low back pain, which will trigger an episode to be measured.
Occupational and physical therapy professionals who are interested in learning about the HCPCS codes that will trigger a Low Back Pain Episode can review the criteria and download the codes on the CMS website about cost measures and development process.
Changes to Quality Measures
Looking ahead to the new year, CMS has done some considerable cleanup of the Quality Measures with a focus on moving clinicians toward MVP reporting. Many of the measures that were removed were topped out—meaning that, according to CMS, “meaningful distinctions and improvement in performance can no longer be made.”
Generally, we see that CMS is moving away from process measures, toward outcome measures. The latter require more information collection and reporting to obtain a performance score.
Additions, Removals, and Improvements
The finalized 2024 measure set includes a total of 198 MIPS quality measures, including 11 new MIPS quality measures, including six high-priority measures, of which four are patient-reported outcome measures (PROMs); and one composite measure; removal of 11 quality measures, partial removal of 3 quality measures, and changes to 59 existing measures.
Choosing Quality Measures in 2024
For a better chance at achieving scoring thresholds, clinicians should avoid topped-out Quality measures in 2024.
Why? Because CMS focuses on incentivizing MIPS participants to use new Quality measures, where they’ve determined that greater performance improvement is possible. When a new measure is introduced, clinicians have the opportunity to obtain between 7-10 measure achievement points, or 5-10 measure achievement points in the second year of the measure. To maximize these achievement points, clinicians must meet the case minimum and data completeness requirements.
Removal of BMI Screening Measure
CMS removed the measure “Q128 Preventative Care and Screening for Body Mass Index (BMI) Screening and Follow up Plan,” and replaced it with Quality measure “Preventative Care and Wellness.” The new measure requires much more information gathering for successful reporting.
Further, Q128 is no longer eligible for reporting in the traditional MIPS Quality category; however, clinicians can still report performance on this measure if reporting using an MVP.
Notable New Measures for PT, OT, and SLP
Rehabilitation clinicians know that finding applicable measures to report on often presents a challenge. We recommend reviewing the following new measures as potential additions for your practice.
Measure 487: Screening for Social Drivers of Health
The measure supports the process of collecting drivers of health data, which is a foundational step towards defining, addressing, and allocating supportive resources to patients in an impactful manner. This measure can be calculated for patients 18 years and older. Patients are screened for food insecurity, housing instability, transportation needs, utility difficulties, and interpersonal safety. This measure can be reported under Traditional MIPS and MVPs.
Measure 498: Connection to Community Service Provider
This measure represents the percent of patients 18 years or older who screen positive for one or more of the following health-related social needs (HRSNs): food insecurity, housing instability, transportation needs, utility help needs, or interpersonal safety; and had contact with a Community Service Provider (CSP) for at least 1 of their HRSNs within 60 days after screening.
Measure 502: Improvement or Maintenance of Functioning for Individuals with a Mental and/or Substance Use Disorder
This measure represents the percentage of patients aged 18 and older with a mental and/or substance use disorder who demonstrated improvement or maintenance of functioning based on results from the 12-item World Health Organization Disability Assessment Schedule (WHODAS 2.0) or Sheehan Disability Scale (SDS) 30 to 180 days after an index assessment.
Measure 503: Gains in Patient Activation Measure (PAM®) Scores at 12 Months
The Patient Activation Measure® (PAM®) is a 10 or 13 item questionnaire that assesses an individual’s knowledge, skills and confidence for managing their health and health care. The measure assesses individuals on a 0-100 scale that converts to one of four levels of activation, from low (1) to high (4). The PAM® performance measure (PAM®-PM) is the change in score on the PAM® from baseline to follow-up measurement.
Alternatives: Specialty Measure Sets and Eligible Measures Applicability
Other options for finding applicable measures are specialty measure sets available for PT, OT, and SLP. These are the Physical & Occupational Therapy Measure Set and Speech-Language Pathology Specialty Set.
Clinicians with limited measure options can use the EMA process. The Eligible Measures Applicability (EMA) process allows reporting fewer than six measures. This is an option for providers who do not have patients eligible for certain Quality Measures.
Changes to the Improvement Categories
CMS’ focus on addressing the social determinants of health and patient access to care is evident in the changes to the Improvement Activities Category, which makes up 15% of the total traditional MIPS score. For the 2024 performance year, CMS added five, changed one, and removed three improvement measures.
Notable Changes to Improvement Measures for Rehabilitation Therapy
PTs and OTs participating in MVPs will have several Improvement Activities reporting options. Improvement Activities include providing education for new clinicians, identifying risks associated with food insecurity and connecting patients to resources, and interoperable clinical decision-making support.
New Improvement Activity Measure: Practice-wide Quality Improvement
Practice-wide quality improvement is an Improvement Activity Measure that can only be reported in an MVP. The measure requires clinicians to create a quality improvement plan within the practice and create a culture in which all staff can participate. Activities include training all staff, promoting transparency, conducting regular meetings, and staff integration.
KX Modifier Threshold for 2024
New KX modifier thresholds have been set. Therapy providers add the KX modifier to claim lines to attest that “services at and above the therapy thresholds are medically necessary, and that documentation in the patient’s medical record justifies the services.”
In 2024, the KX modifier threshold for combined physical therapy and speech-language pathology is set at $2,330. The occupational therapy threshold is set at $2,330 as well. This marks an increase from $2,230 (for both) in 2023.
New: Caregiver Training Services Codes
CMS recognizes that caregiver training is a reasonable and necessary component of care, especially when the patient may require assistance in carrying out the treatment plan. Therefore, Medicare Part B will now reimburse rehabilitation providers for Caregiver Training Services (CTS) to allow PTs, OTs, and SLPs to bill for caregiver training without the patient being present. Caregiver is defined as a family member, friend or a neighbor.
The Caregiver Training Services codes (97550, 97551, 97552) will allow clinicians to bill for caregiver training for patients with an active treatment plan.
Telehealth Services Continue for Rehab Therapy
Telehealth will remain an option for the delivery of PT, OT, and speech therapy services in 2024, thanks to a temporary extension provided by the Consolidated Appropriations Act of 2023. Telehealth is defined by CMS as the use of two-way, real-time audio and video telecommunications.
This is a win for those who have seen the many benefits of telehealth in PT, OT, and SLP practice, but further research and advocacy within the field will be required to institute telehealth as a permanent service offering.
General Supervision Updates for Physical Therapy and Occupational Therapy Assistants
Remote Therapeutic Monitoring in Private Practice
Remote Therapeutic Monitoring (RTM) refers to the use of a device to monitor a patient’s response to treatment. In 2023, CMS finalized policies to allow for RTM services to be furnished by PTs and OTs under general supervision. In the 2024 Final Rule, OTs and PTs may use general supervision to bill for RTM services monitored by therapy assistants. In this context, the OT or PT does not have to be immediately available during the RTM services.
Supervision Policy for OT and PT in Private Practice
Although CMS modified the supervision rules to allow general supervision of therapy assistants by OTs and PTs for remote therapeutic monitoring services (RTM), the supervision rules were not changed for therapy assistants in private practice.
This means that OTs and PTs must continue to provide direct supervision of therapy assistants in private practice, during which the supervising clinician must be immediately available during treatment sessions.
CMS is soliciting comments on the impact of quality of care and will consider changes to supervision in future rule-making. Visit the QPP feedback page for more information.
Policies for Third Party Intermediaries
If your practice works with a third party entity to submit data for any of the MIPS performance categories, pay attention to this change. In 2024, third party intermediaries have to be a QCDR or qualified registry to submit data to CMS, which cited data inaccuracies in previous reporting periods.
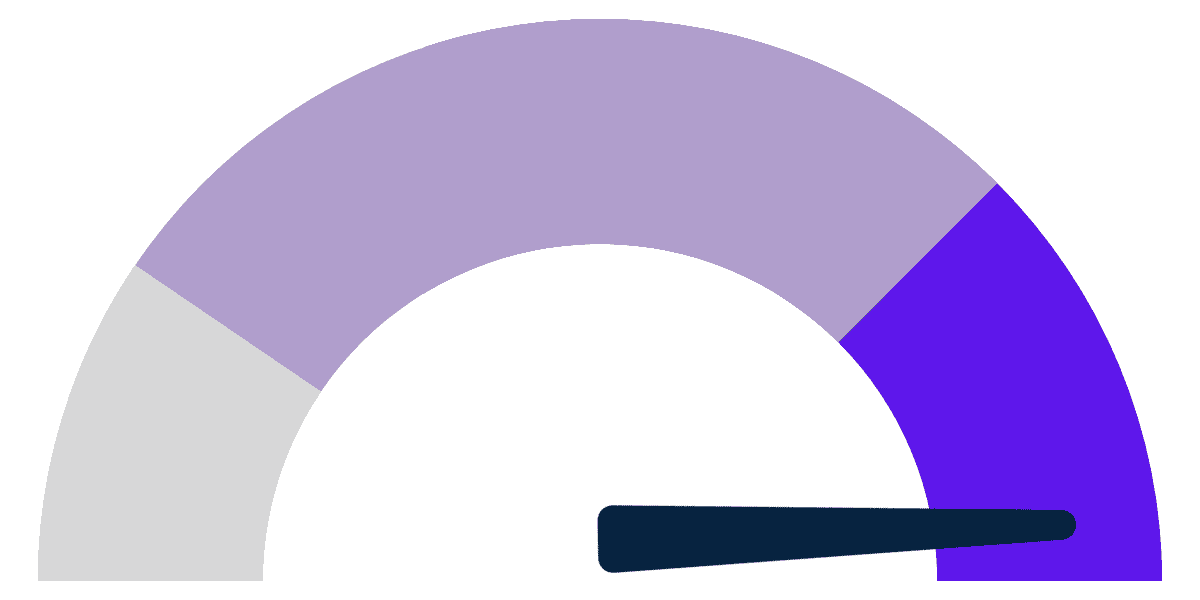
Meeting the MIPS Threshold in 2024
With a declining conversion factor, it’s more important than ever to protect and improve your Medicare Part B revenue. Future-focused clinicians and practices will want to maximize the chance of reaching the MIPS threshold and receiving a positive payment adjustment.
Use this calculator to estimate how your MIPS score
could affect revenue in the next payment year.
Payment years are two years after the reporting year, i.e. a MIPS score for the 2024 performance year will affect payments in 2026.
Within the
Lowest Quartile
Below the MIPS
Meets or Exceeds the
Performance Threshold
How are MIPS scores calculated?

$
A positive adjustment could bring your $
───
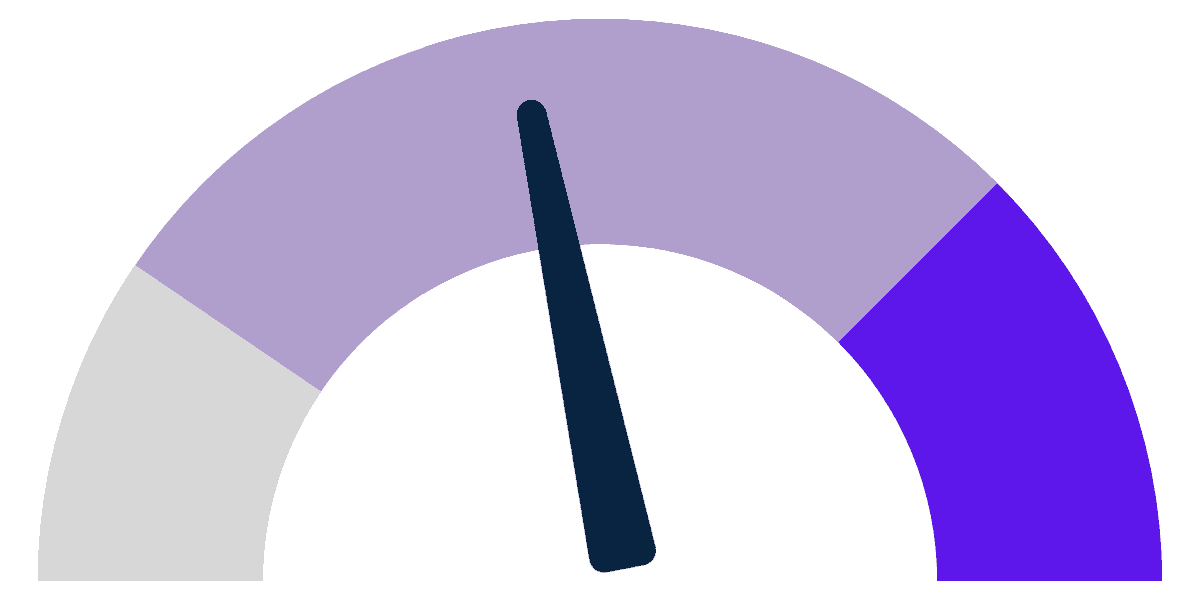
NEUTRAL ADJUSTMENT
If your MIPS score equals 75 points exactly, your Medicare Part B payments won't receive an incentive nor disincentive. Your revenue would remain at $
───
2024 UPDATE
For rehabilitation therapists who participate in MIPS, the 2024 Final Rule now requires reporting in the Promoting Interoperability performance category (25 points, or 25% of the total MIPS score).
The PI category requires use of certified EHR technology (CEHRT) for 180 days out of the 2024 performance year.







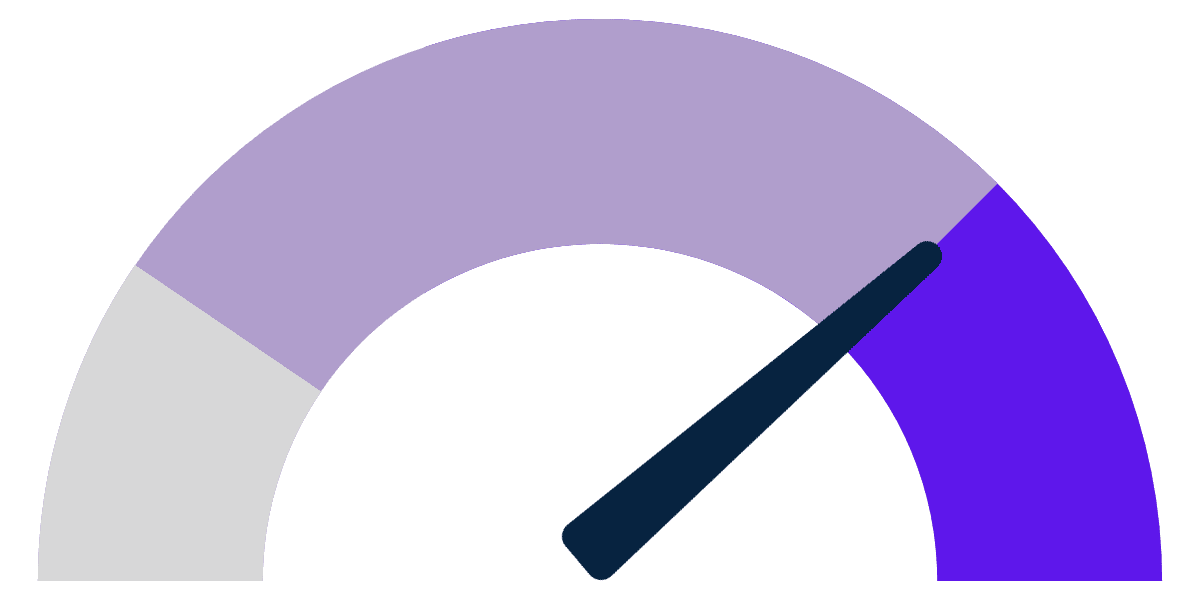
As long as your score is above 18.75, you aren't guaranteed to receive the maximum negative penalty... But you could still see your hard-earned revenue fall by
- $
The range of adjustment could see $
───
2024 UPDATE
For rehabilitation therapists who participate in MIPS, the 2024 Final Rule now requires reporting in the Promoting Interoperability performance category (25 points, or 25% of the total MIPS score).
The PI category requires use of certified EHR technology (CEHRT) for 180 days out of the 2024 performance year.
If you're not using a certified EHR and want to maximize your chance of a positive adjustment, it's time to consider a switch. Raintree is the only certified EHR designed specifically for PT, OT, SLP, and multi-specialty practices.







If your MIPS score equals 75 points exactly, your Medicare Part B payments won't receive an incentive nor disincentive. Your revenue would remain at $
POSITIVE ADJUSTMENT
With a score above 75 points, you would exceed the MIPS threshold and receive an incentive capped at 9%. Your projected revenue could see a boost of $
DOWNWARD ADJUSTMENT
With a score below 75 points, you would not meet the MIPS threshold. With the maximum penalty (-9%), your revenue would fall by - $
───
2024 UPDATE
For rehabilitation therapists who participate in MIPS, the 2024 Final Rule now requires reporting in the Promoting Interoperability performance category (25 points, or 25% of the total MIPS score).
The PI category requires use of certified EHR technology (CEHRT) for 180 days out of the 2024 performance year.
If you're not using a certified EHR and want to maximize your chance of a positive adjustment, it's time to consider a switch. Raintree is the only certified EHR designed specifically for PT, OT, SLP, and multi-specialty practices.







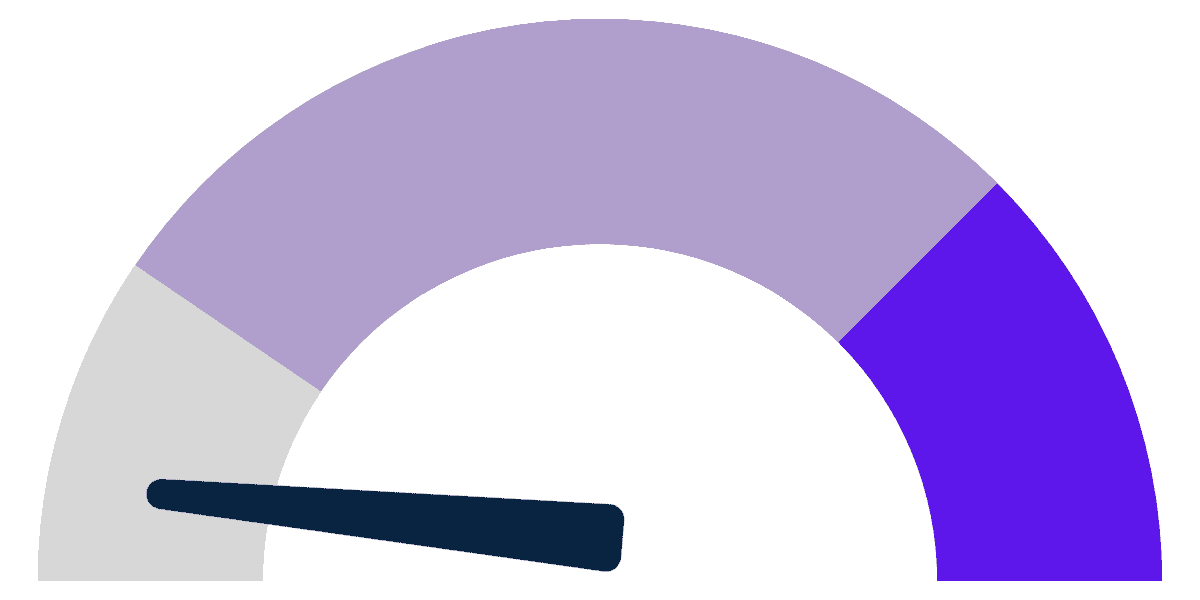
This means you would see your hard-earned revenue fall by
- $
───
2024 UPDATE
For rehabilitation therapists who participate in MIPS, the 2024 Final Rule now requires reporting in the Promoting Interoperability performance category (25 points, or 25% of the total MIPS score).
The PI category requires use of certified EHR technology (CEHRT) for 180 days out of the 2024 performance year.
If you're not using a certified EHR and want to maximize your chance of a positive adjustment, it's time to consider a switch. Raintree is the only certified EHR designed specifically for PT, OT, SLP, and multi-specialty practices.







Offering the only ONC-certified EHR software designed for rehabilitation therapy, Raintree Systems is here as your partner in long-term growth. Experience the future of rehab therapy with Raintree.
As a reminder: In order to meet the MIPS Promoting Interoperability requirements in 2024—25% of the total score—you need to demonstrate use of CEHRT for 180 days within the performance year.
If you’re not already using a certified EHR, time is short. Implementing a new system doesn’t happen overnight. Schedule a demo with Raintree, today.

Veda Collmer, JD, CIPP/US, Raintree Systems’ General Counsel, Chief Compliance Officer, brings more than 10 years of experience in health law, privacy and compliance. Veda received the Robert Wood Johnson Foundation Public Health Law Fellowship in 2012 and completed her fellowship at the Arizona State University Sandra Day O’Connor College of Law.
- With contribution from Kathryn Rigda, PT (Director, Product Management) and Kaitlin Beal (Senior Project Manager).