Imagine trying to renovate an old house with outdated wiring and a deteriorating foundation. No matter how much paint you splash on the walls or modern furniture you bring in, the underlying issues will inevitably cause problems. It’s just a matter of time.
This scenario is strikingly similar when it comes to using legacy EMR (electronic medical record) software. Just like a stable and modern infrastructure is critical for a comfortable and safe home, using modern software is essential for efficient, effective, and high-quality patient care.
So, is your chosen system built to last? Or is it time to go full-on Extreme Makeover: Tech Edition? In this blog, we’ll unravel the distinctions between legacy technology, established solutions, startups, and more.
Legacy EMRs and Systems: Definition and Misconceptions
When you hear the word “legacy,” what comes to mind? You might think of a valuable keepsake passed through the generations, or a person’s reputation after a life well-lived.
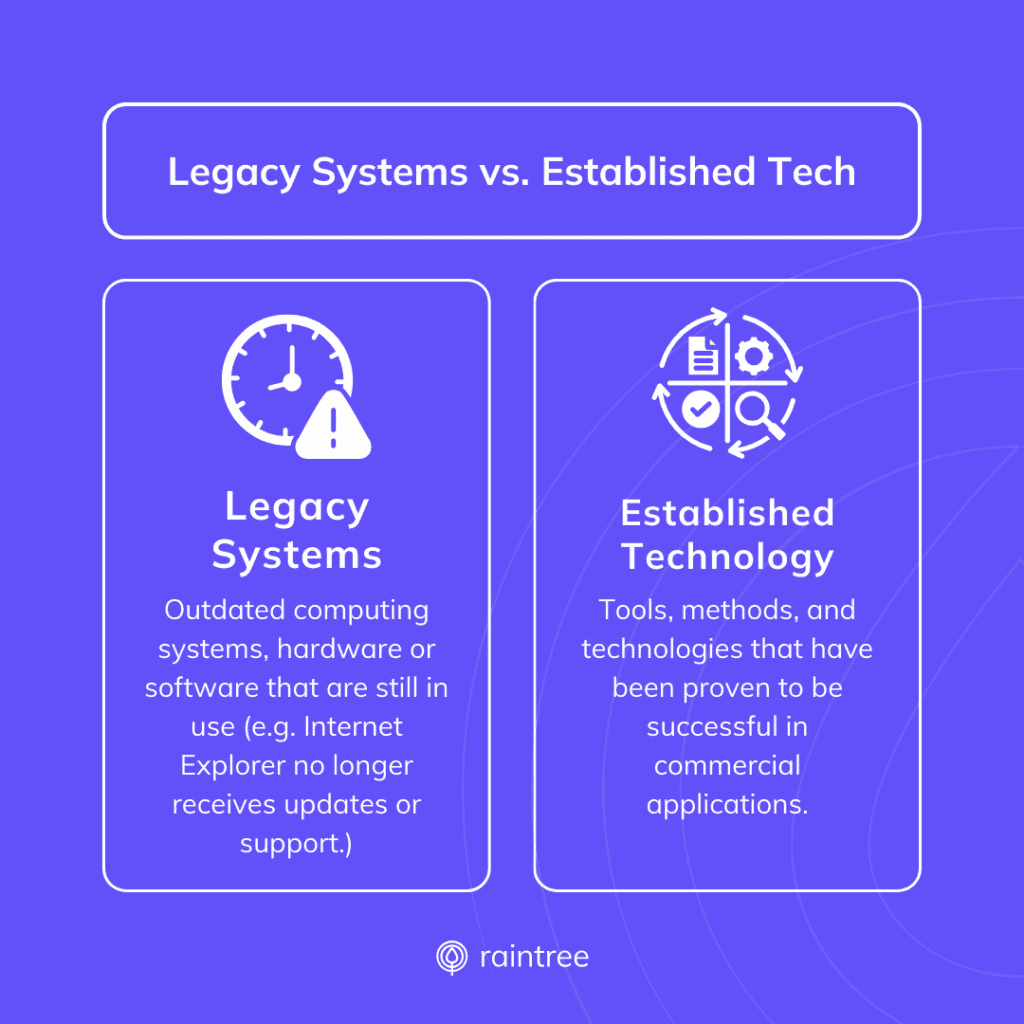
However, in the context of technology, “legacy” often translates to: Outdated. Broken. Difficult to manage. But the truth is that being long-established does not mean your software is falling short. Let’s explore the real definition of a legacy system.
What Is a Legacy System?
TechTarget defines a legacy system (or legacy application) as “any outdated computing system, hardware or software that is still in use.” They point to the red flags of legacy IT, when systems are:
🚩 Abandoned. The technology no longer receives updates or support from its developers.
🚩 Off the market. The systems or applications are no longer available for purchase.
🚩 Obsolete or siloed. Maintenance, repairs, or integrations may be difficult or impossible.
🚩 Vulnerable and non-compliant. They can’t meet modern data security standards.
Established and Evolving Systems
In contrast, a longstanding system with a rich history may actually be the result of continuous improvement and evolution. These systems are:
✅ Well-established. Both the business and its software have been tested over time and have proven reliable and effective.
✅ Continuously updated. These systems receive regular updates with new features, fixes, innovations, and integrations.
✅ Adaptive. They should provide a future-focused product roadmap that’s responsive to client feedback, industry trends, and regulatory updates.
✅ Resource-backed. The software is supported by a wealth of experience, knowledge, and often a significant investment in ongoing development and improvement.
This distinction is vital in a field like healthcare, where quality patient care is dependent on reliable and efficient software. It’s not just about adopting the bells and whistles of new technology; it’s about the integrity, dependability, and scalability of the platform over time.
System Selection and Decision-Making Strategies
The process of choosing a new EMR or practice management software involves assessing the organization’s needs, resources, and long-term goals. With various technology options available, selecting the right digital backbone can be a daunting task. Here are a few ways that practices tackle their technology needs:
In-House Solutions
Some practices have the resources and vision to build and maintain their own software. Here, the advantage is clear: complete control over the system’s form and function.
However, the investment in time, money, and expertise to create and support these systems can be substantial. In-house (or “home-built”) solutions risk becoming siloed from industry-standard advancements, and may incur an ongoing cost that’s easily underestimated. Though they may be the best choice for limited or short-term solutions, maintenance becomes increasingly complicated with growth and may present compliance risks.
Integrated Systems
Other practices use a combination of best-of-breed tools, which integrate to form a bespoke solution.
This patchwork of systems often includes an EMR along with specialized tools for billing, scheduling, telehealth, et cetera. Choosing a variety of tools has its perks, like third-party support, regular updates, and lower costs up front. On the other hand, too many systems creates an increasingly complicated infrastructure to maintain. Workflows can become disjointed if the integrations between two systems cause lags, require manual workarounds, or lead to failure.
All-in-One Platforms
At the other end of the spectrum are all-in-one platforms that merge EMR, practice management, and additional tools into a single interface.
Finding a unified solution can provide many benefits, but the main appeal is efficiency. When multiple domains of your practice—from front office, to clinical, to back office processes—utilize a single platform and database, it’s possible to collaborate more quickly while keeping your team up-to-date and on the same page. Additionally, working with a centralized solution means fewer vendors to manage (because no one wants a software experience to feel like herding chickens).
The potential downside includes the risk of “vendor lock-in”—when your platform hinders your growth, but migrating to a new system is prohibitively complicated or expensive. So it’s especially important to make sure you’re choosing a solution that can grow and scale alongside your practice over time.
EMR Startups and Emerging Technology: Pros and Cons
So, now that you know a bit more about your tech stack options, and you know what a legacy system is (or isn’t), you might wonder: What about newcomers to the EMR space?
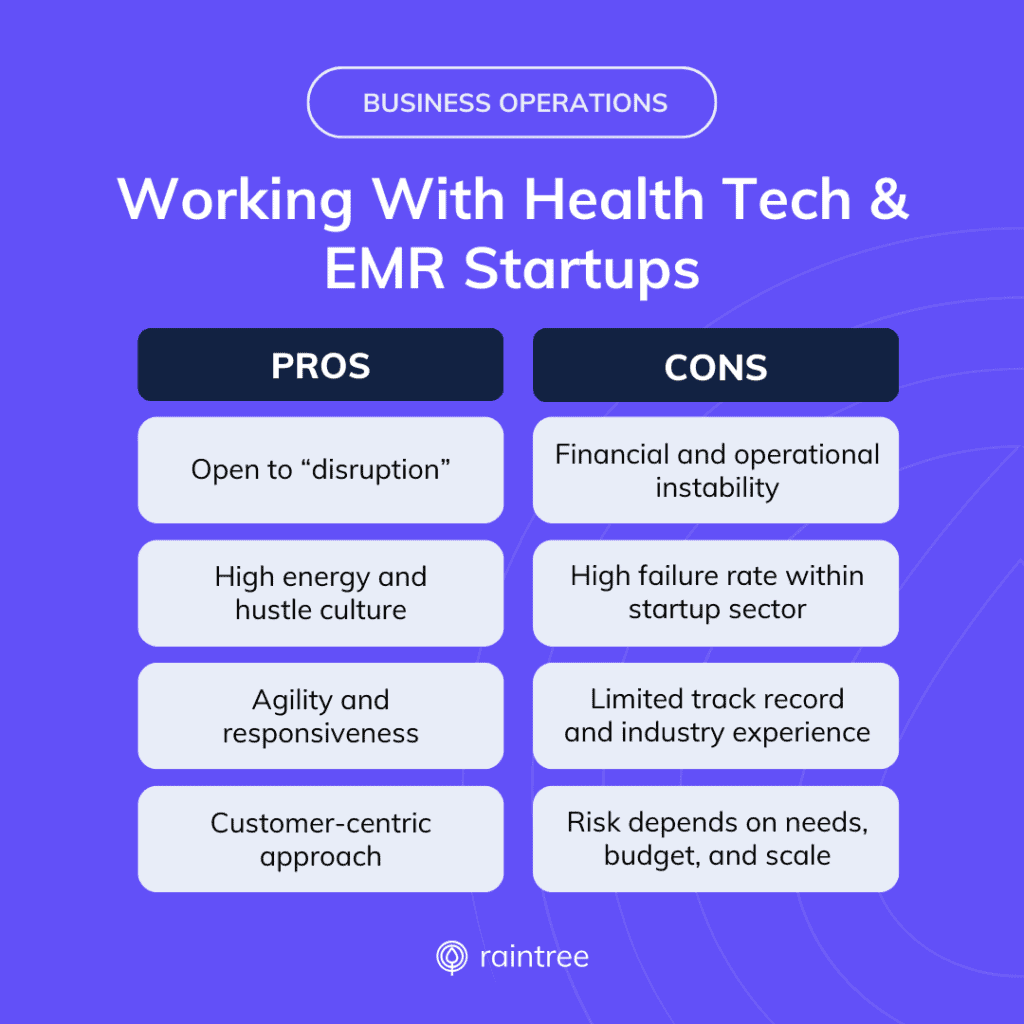
Startups are typically thought to be the nexus of tech innovation. They’re all about the hustle, looking for ways to “disrupt” the status quo with fresh and flashy solutions—and that energy can be contagious. Additionally, startups are often associated with agility and a customer-centric approach.
Still, working with a startup can present its own challenges, like financial and operational instability. Startups in the health tech space have a high failure rate, with few outlying unicorns. Healthcare organizations and practices must decide how much risk to take on, which may vary based on your needs, budget, and the maturity and scale of your operations.
How to Find Industry-Proven Solutions
For outpatient therapy practices, selecting an EMR system is never a simple decision—but always an important one. This is a business partnership, and your chosen partner should support your business growth, enable clinical and operational efficiency, protect patient data and safety, and elevate overall user experience.
That’s why, in contrast to working with a startup or building an in-house solution, partnering with an “industry-proven” vendor has its perks. When you’re looking for a new EHR or EMR, seek well-established companies that can demonstrate:
- Industry-specific knowledge. This will come through in the solution’s specialized features, workflows, and best practices—as well as the accumulated years of expertise among its engineering, design, and support teams.
- High performance. Look for solutions that are trusted by top players in your field, as well as measurable results and recommendations shared by practices like yours.
- Security standards. Patient safety and clinical data security are top priorities.
- Thought leadership. These solutions are often ahead of the game, anticipating and adapting to new industry needs and regulatory developments.
The true gold standard is not just an EMR that works for today, but a solution that demonstrates a commitment to your future state.
The Last EMR You'll Ever Need
Let’s return to that idea from the very beginning. When you’re in the market for a house, it’s easy to see the promise and potential of a fresh new property, or the charm of a historic building. But what you’re looking for, in the end, is a new home. One where you can be at ease, provides stability and security, and is built on good bones. A place where you can grow.
Similarly, if you’re tired of outgrowing your EMR systems, it may be time to find your long-term solution. One that delivers proven results and a future-proof foundation.
A legacy system, as we’ve established, can hold you back. But longevity is a testament to the evolving competence and enduring value of any health IT solution.
Raintree Systems helps physical therapy, occupational therapy, speech-language pathology and multi-disciplinary practices grow and succeed with scalable and robust software. Raintree offers the only ONC-certified EHR system designed specifically for rehab therapy. Want to learn more? Schedule a demo and learn why high-growth PT, OT, SLP, and multi-disciplinary practices choose Raintree.
Frequently Asked Questions
What are some examples of legacy systems or applications?
Legacy systems or applications run on outdated computing system, hardware or software. Types of legacy systems could include:
- Aging database systems or infrastructure.
- Sunsetted products (e.g. Internet Explorer, which stopped receiving support in 2022).
- Out-of-date device operating systems.
- In-house or custom-built software, developed by a business to support internal operations but no longer viable, scalable, or secure.
Why would a healthcare practice choose to use a legacy system or EMR?
There are several reasons why a company might opt to continue using a legacy EHR or system despite its limitations, including:
- Cost. Upgrading to new technology can be expensive, involving not just the purchase of new software or hardware, but also the costs associated with training employees, legacy data migration, and potentially disrupting operations during the transition period.
- Importance to business operations. Some legacy systems may operate critical business functions that are deeply integrated into the company's workflow, making the risks and potential downtime of transitioning daunting. Legacy systems might also have custom features specifically tailored to the organization's unique needs, which new solutions may not readily replicate.
- Hesitance. Perceived lack of suitable alternatives can make organizations resistant to move away from what they know works, even if it's outdated or holding them back from their next stage of growth.
What is the process of transitioning from a legacy EHR to a new EMR?
Transitioning from a legacy EMR system to a new platform involves several critical steps:
- Assessment and planning. Evaluate current system capabilities and limitations, set clear objectives for the new system, and create a detailed transition plan.
- Vendor selection. Research and select an EMR vendor that aligns with your practice's needs, budget, and long-term goals.
- Data migration. Securely transfer legacy patient data and health information from the old EMR to the new platform, ensuring data integrity and compliance with privacy regulations.
- Training and implementation. Provide comprehensive training for staff to get acquainted with the new system and implement the EMR in phases to minimize disruptions.
- Testing and optimization. Conduct thorough testing to identify and address any issues, and continuously optimize the system based on user feedback and performance metrics.
- Ongoing support. Establish a support structure with your EMR vendor for troubleshooting, updates, and future enhancements.
What is the failure rate of health tech startups?
Some estimate the rate of failure for startups is above 90%. This stat is based, in part, on a widely-cited 2019 Global Startup Ecosystem Report, which stated that only 1 in 12 startups will succeed. Others look to new business failure rates. For example, the U.S. Bureau of Labor Business Employment Dynamics report shows a 70% failure rate within 10 years. Top reasons for startup failure include running out of capital, lack of industry need, competition, unsuccessful business models, and regulatory challenges.