Whether due to a chronic condition, stroke, injury, age-related changes, or swallowing difficulties, Medicare recipients often need speech therapy. There’s no shortage of speech-language pathologists (SLPs) who are more than ready to step in to support older adults and individuals with disabilities. That’s good news for the more than 65 million Medicare beneficiaries in the U.S. today.
But Medicare billing is a whole different story. It’s complicated. It changes regularly. And it takes focus and expertise to master. We’ve developed this guide to cover essential facts about speech therapy billing and Medicare to make your job just a little bit easier.
Speech Therapy and Medicare Coverage
The first thing to know about Medicare is that there are four types, called Part A, B, C, and D.
Here’s a brief rundown of what those terms mean.
Medicare Part A ties to treatments received in a hospital or inpatient care facility. If a patient in a hospital or inpatient rehabilitation center needs speech therapy, it may be covered under Medicare Part A.
Medicare Part B covers costs for therapy in an outpatient setting. This may include an SLP’s office, outpatient clinics, or outpatient care received at a hospital.
Medicare Part C includes Medicare-approved plans provided by private insurers.
Medicare Part D is an optional outpatient prescription drug benefit.
If you’re an SLP who provides at least some outpatient care under Medicare Part B, you must enroll as a Medicare provider and bill Medicare for any services provided to eligible beneficiaries.
Speech Therapy Services Under Medicare Part B
SLPs treat a wide range of conditions that affect patients across their lifespans. Some of the more common conditions SLPs address for Medicare patients include:
Aphasia: Difficulty with speaking, understanding, reading, and writing caused by damage to language center in the brain.
Dysarthria: Difficult-to-understand speech caused by diminished motor coordination of the muscles used for speech.
Apraxia of speech: Speech difficulties that emerge when the brain has difficulty coordinating the movements needed for speaking.
Dysphagia: Swallowing disorders that can impact the ability to chew and/or move food through the mouth or throat.
Cognitive-communication disorders: Communication difficulties caused by cognitive impairments.
Traumatic brain injury (TBI) related difficulties: Communication or swelling difficulties caused by damage to the brain.
Parkinson’s disease related difficulties: Speech and language differences that arise due to Parkinson’s disease, such as imprecise articulation or monotone voice.
Oral motor disorders: Difficulties associated with coordination of muscles used for speech, chewing, or swallowing.
Coverage for Speech-Language Pathology Services
Coverage for the conditions treated by speech therapy can vary by location. Why? Each region has its own Medicare Administrative Contractor (MAC), which is a private government contractor charged with managing Medicare claims in a specific locality. Your regional MAC handles all the Medicare claims in your area and makes Local Coverage Determinations (LCD) about what to cover in your jurisdiction.
Sometimes, you may hear from a therapy colleague in another part of the country (through social media, for example) that Medicare covers a certain treatment or condition. But unfortunately, that may not be true for your practice. LCDs are not consistent from region to region. Instead of relying on the grapevine to deduce what’s covered, your best bet is to get familiar with the LCD guidelines put forth by the MAC in your area.
Who Can Provide Speech Therapy Under Medicare?
Federal law clarifies what credentials clinicians need to qualify as Medicare providers. To qualify as a speech therapist, you need to have either earned a license through your state or achieved a relevant certification in states without licensure. The American Speech-Language-Hearing Association (ASHA) Certificate of Clinical Competence (CCC) is one example of a qualifying credential.
That said, SLP assistants, students, and clinical fellows can provide some services under Medicare Part B. In such cases, a qualified practitioner must be present in the same room throughout service delivery. The qualified practitioner must supervise the services and maintain total responsibility for any assessments and treatments.
Requirements of Treating Medicare Beneficiaries
Under Medicare, either a physician or an SLP may establish a plan of care for speech therapy. And Medicare patients do not need a physician’s referral to start therapy with an SLP. However, there is an important caveat. The patient’s physician must certify any plan of care created by an SLP within 30 days for any patient receiving outpatient therapy. Further, physicians must recertify plans every 90 days after the start of treatment or whenever there is a significant plan modification. For comprehensive rehabilitation facilities or home health agencies, a physician must review care plans every 60 days.
As a Medicare provider, you may need to participate in the Merit-based Incentive Payment System (MIPS). The MIPS program aims to incentivize and reward Medicare providers to deliver high-quality care. The requirement to participate in MIPS typically kicks in if you bill more than $90,000 per year (called the “low-volume threshold“) under Medicare Part B. If you take part in MIPS, you can receive a payment bonus for consistently delivering top-notch service. On the flip side, moderate or subpar service can result in no payment adjustment or even a payment penalty.
Medicare Billing for Services Outside the Clinic
As a therapist or practice owner, you may not want to limit your practice to outpatient facilities. Under Medicare, that’s possible, but it may require a little extra legwork.
Medicare allows you to provide services to homebound patients. This means the patient has difficulty leaving home without some kind of assistance, either from a person or a medical device, such as a wheelchair or walker. Alternatively, a physician may recommend that certain patients stay at home due to specific conditions.
SLPs may also provide services to covered Medicare beneficiaries in school settings and offer telehealth. When providing services in alternate settings—like homes, schools, or online—you may need to follow special coding and documentation requirements.
Speech Therapy Billing and Medicare: Best Practices
The federal agency that manages Medicare, the Centers for Medicare and Medicaid Services (CMS), has a big responsibility to use public funds in the best interest of the nation and its people. CMS must prevent fraud, waste, and abuse to the best of its ability. That’s a big reason why Medicare billing is full of intricacies and nuances.
To the uninitiated (or even those who’ve managed medical billing for years), every Medicare claim can seem like it requires jumping through many hoops. It’s true, but you can make the process more efficient by following proven Medicare billing best practices.
Provide Defensible Documentation
Let’s be honest: Documentation is rarely a therapist’s favorite part of the job. But it’s an necessity for effective speech therapy billing and Medicare reimbursement.
Why? Your documentation must stand up to scrutiny and meet exacting standards set forth by CMS. It needs to outline the patient’s medical history, detail any assessments you conduct, and include a thorough treatment plan. It must justify the patient’s medical need for therapy and clarify why your skilled intervention was necessary.
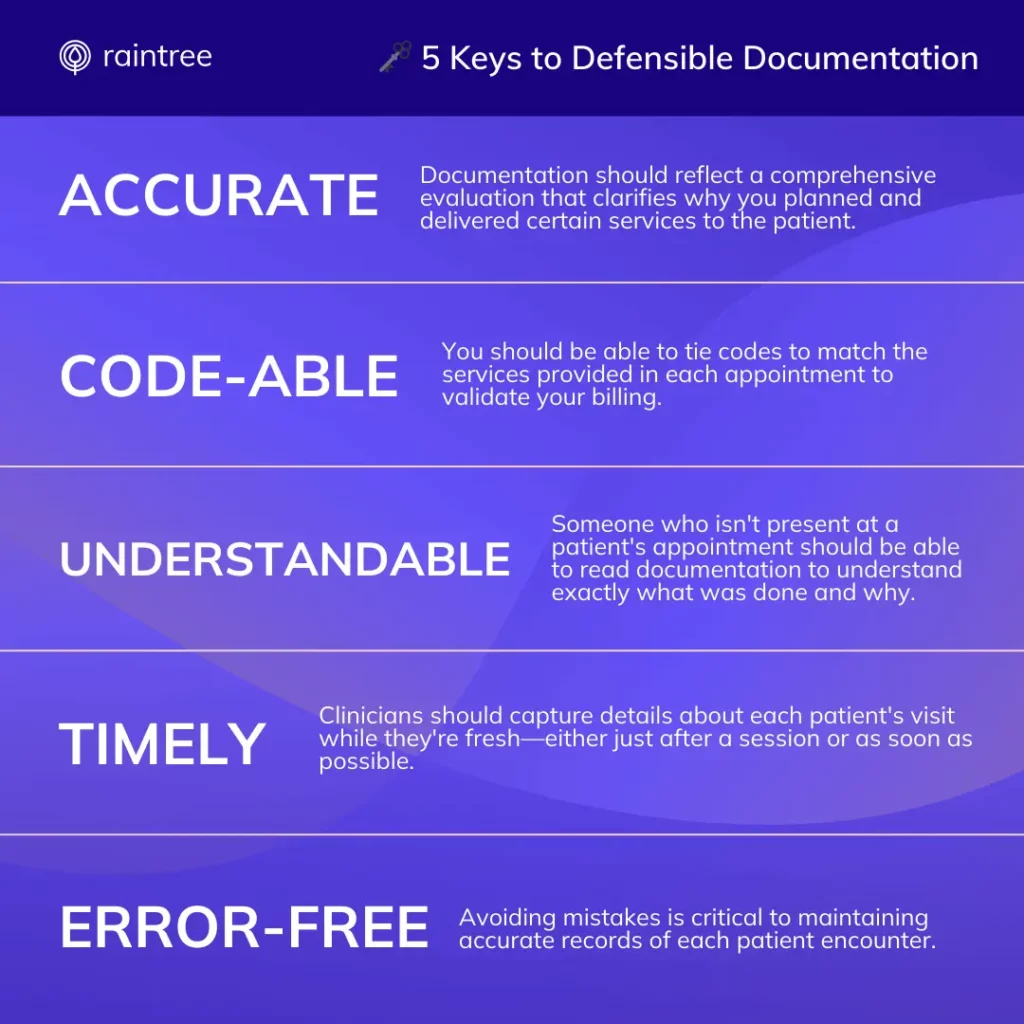
To help you develop high-quality, defensible documentation, ASHA created the handy ACUTE mnemonic that stands for: Accurate. Code-able. Understandable. Timely. Error-free.
Mastering SLP Billing Codes and Modifiers
Every medical bill includes at least one CPT code—a sequence of characters that identify procedures and services provided by qualified healthcare practitioners. There are thousands of medical codes, but you’ll only use a small fraction of them as an SLP.
You may also use certain code modifiers, which are two digits appended to codes that provide more information. For example, there is a specific modifier (GN) that identifies speech therapy services delivered under an outpatient plan of care. Other modifiers may indicate care provided via telehealth. And there are others that may be relevant to your services. Another modifier you’ll likely encounter is KX. This modifier indicates that a patient has met his or her annual Medicare Part B cap but that the clinician deems additional services medically necessary.
Medicare Threshold for Outpatient Speech Therapy
Why are modifiers like this important? Speech-language and physical therapy services are grouped under the same Medicare cap (unlike occupational therapy, which has its own limit). Through 2028, the combined threshold for the two disciplines is $3,000. However, once those services hit $2,230, you’ll need to start using the KX modifier to designate ongoing medical needs. Note that after 2028, the annual limit will be updated annually to align with the Medicare Economic Index (MEI).
Importantly, just because you can continue to provide skilled therapy services to a patient doesn’t mean that you should. You need to be able to justify that a patient’s condition will improve within a reasonable amount of time. In cases of patients with degenerative conditions, you need to validate that continued speech services are necessary for the patient to maintain a level of functioning.
💯 Practical Advice
There’s a lot more to know about codes and modifiers. Our resource on the Most Common Codes and Billing Modifiers, is an excellent place to start.
Avoid Billing Errors (and Denied Claims)
In life, mistakes happen. In Medicare billing, even the simplest misstep can lead to denied claims and months of working to get the payment you deserve. Plus, if you make too many mistakes, that can raise a red flag with CMS or lead to an unwelcome fraud investigation. You definitely don’t want that to happen!
How can you protect yourself? First, you should know that manual processes are one of the biggest causes of speech therapy billing and Medicare errors. It’s all too easy to submit a bill with a typo or an inaccurate code. Insufficient documentation or omission of necessary services are other common roadblocks.
To save yourself some headaches (and get paid faster), you should familiarize yourself with some of the most common reasons for claims snafus. Our resource Top 3 Reasons for Claims Denials reviews three top billing roadblocks and how to prevent them.
Navigate the Intricacies of Speech Therapy Billing and Medicare with Confidence
Medical billing isn’t easy, but you can lean on experts to guide you. You can also choose billing technology that is purpose-built for rehabilitation therapists to automate and streamline essential tasks.
At Raintree, we’ve engineered our revenue cycle management (RCM) and billing solutions with the unique needs of therapists like you in mind. Our software coordinates every step of the process—from initial insurance verifications through clinical documentation to billing, claim management, and collections.