Home exercise programs (HEPs) play an important role in recovery for physical therapy and rehabilitation patients, but getting them to follow through with a prescribed plan often poses a challenge. Despite the benefits of an HEP, studies have found that non-adherence for musculoskeletal (MSK) conditions can be as high as 65%.
For growing or large-scale rehab therapy organizations, the stakes are especially high. Low HEP compliance not only impacts individual outcomes—it affects clinic efficiency, clinician bandwidth, and the organization’s ability to deliver scalable, consistent care. To address this, organizations must tackle both the patient-level and system-wide factors driving non-adherence.
Understanding Barriers to HEP Adherence
Rehab therapists put a lot of time and effort into developing HEPs, but even the best-designed plan can fall short if patients don’t follow through. Identifying the common barriers to home exercise program compliance is the first step toward creating individual and organization-wide adjustments.
Why Patients Don't Follow Home Exercise Programs
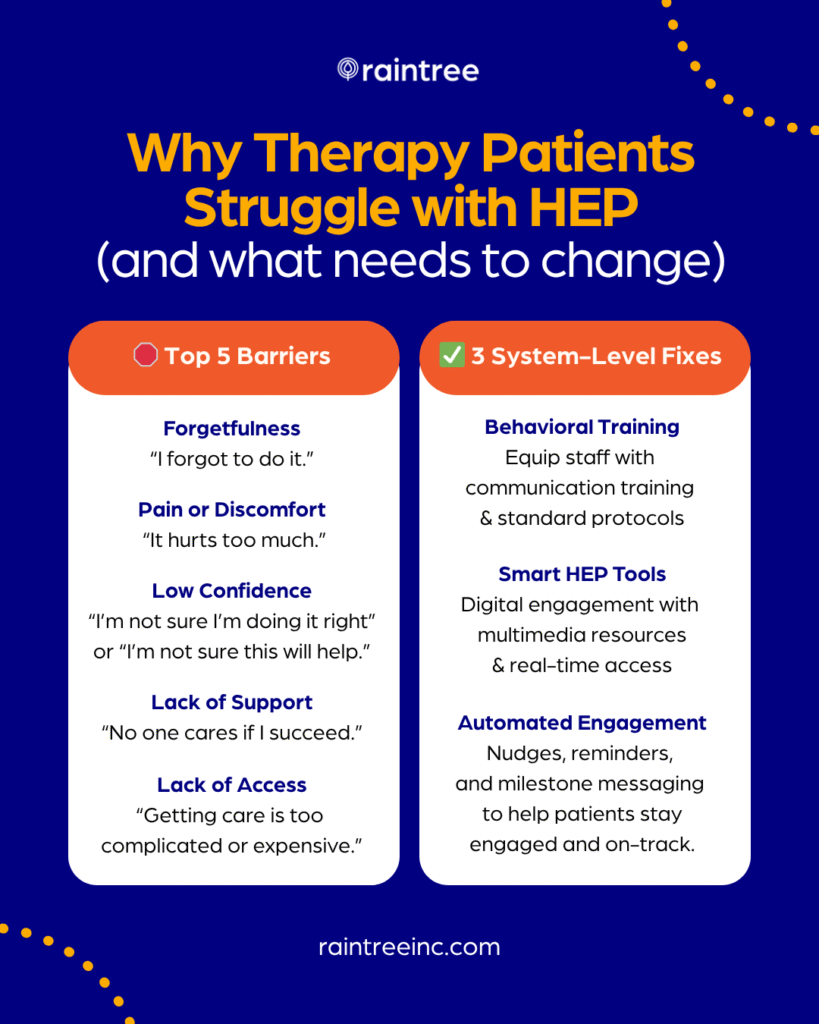
Patients often face several personal challenges and perceived barriers that can make adherence to prescribed home exercise programs difficult, including:
- Unclear Instructions. Vague guidance or poor visuals lead to errors.
- Overwhelming Complexity. Too many or too difficult exercises discourage follow-through.
- Low Confidence. Patients doubt their ability to perform exercises correctly.
- Lack of Motivation. Without visible short-term progress, patients lose interest.
- Environmental Constraints. Time, space, support, and socioeconomic factors all play a role.
💯 By the Numbers
Physical therapists cite pain, forgetfulness, time constraints, and low self-efficacy as patients’ most frequent barriers to compliance.
Organizational Hurdles in HEP Compliance
For multi-clinic organizations, internal processes and structural limitations can inadvertently contribute to low HEP compliance rates in the following ways:
- Inconsistent Clinical Execution. Variability across clinicians or locations leads to uneven patient experiences and prevents practices from being able to deliver quality care at scale.
- Fragmented Tech Stack. Limited integrations between HEP tools and existing Electronic Medical Records (EMRs) or practice management systems creates data silos, making it harder to operate efficiently or monitor patient progress.
- No Clear KPIs. Without systems to track patient engagement with HEPs alongside clinical progress, organizations struggle to objectively measure adherence rates and correlate them with functional outcomes.
- Disjointed Patient Experience. Lack of standardization in follow-up and support erodes patient trust and engagement.
Recognizing these intertwined challenges makes clear the need for targeted, effective strategies that address both individual patient needs and systemic improvements.
4 Strategies to Scale HEP Success Across Your Organization
Many therapists already excel at boosting patients’ exercise adherence. They achieve this through personalized communication, thorough patient education, active listening, and tailoring exercises to unique patient circumstances and preferences.
While this personalized care is essential, achieving widespread, consistent success across a large outpatient therapy organization requires operationalizing best practices. True scalability and impact come not just from individual clinician brilliance, but from systemic consistency. Here are some strategies to standardize and streamline HEP delivery across multiple clinic locations.
1. Equip Clinicians to Foster Patient Empowerment
Ultimately, HEP compliance hinges on patient buy-in. Disparate approaches to HEP assignment and delivery can lead to confusion or frustration, and ultimately lead to inconsistent outcomes across your network of clinics.
Here are strategies practices may consider to equip therapists to succeed and reduce variability in the patient experience:
- Create a Centralized HEP Protocol. Establish best practices for assigning and demonstrating HEPs. Use a standardized exercise library with room for customization to maintain brand consistency while honoring clinical judgment.
- Train for Consistency. Provide ongoing training in communication techniques, patient education, and motivational interviewing to ensure every clinician reinforces the “why” and “how” of the HEP in the same effective way.
- Operationalize Simplicity. Encourage a “less is more” philosophy: assigning fewer, high-impact exercises shown to improve compliance and patient confidence.
💼 Employer Branding
Beyond training and setting high standards, creating a strong employer brand is a strategic way to attract and retain skilled physical and occupational therapists—fueling consistent, high-quality patient care.
2. Implement a Digital Home Exercise Plan
Technology should scale clinician expertise—not create more work. The benefits of integrating a digital HEP program with your EMR include:
- Multimedia Education. Videos, illustrations, and written instructions reduce confusion and increase patient self-efficacy.
- Anywhere, Anytime Access. Mobile apps make it easier for patients to integrate HEPs into their routines.
- Data Capture & Insights. Track completion, engagement, and feedback to identify at-risk patients and refine care delivery.
💡 Key Takeaway
Digital HEP interventions are shown to increase therapy home exercise adherence and confidence in treatment.
3. Systematize Engagement and Follow-Up
Consistent follow-up is essential—but hard to maintain without systems in place. Large therapy organizations benefit from scalable engagement strategies that ensure patients stay supported between visits.
- Automate Touchpoints. Use reminders, emails, and in-app nudges to keep patients on track—without overloading staff.
- Unified Messaging Strategy. Ensure patients receive the same core messages, support instructions, and tone of care across every touchpoint.
- Engage the Support Network. For some patient populations, it can be helpful to standardize procedures for involving family members or caregivers in understanding and supporting the HEP.
💡 Key Takeaway
Research shows that including digital interventions, including mobile applications and reminders, in home exercise program delivery can positively impact short and long-term exercise adherence.
4. Use Data to Drive Continuous Improvement
Large organizations have an inherent advantage in data collection. Tapping into this wealth of information can provide insights into HEP compliance trends and areas for improvement. To do so:
- Track What Matters. Monitor exercise completion rates, platform engagement, and correlation with functional outcomes.
- Benchmark Performance. Identify high-performing clinicians and clinics, then replicate their success strategies system-wide.
- Close the Feedback Loop. Use real-time data to inform clinical decisions, adjust workflows, and continuously optimize the patient journey. Analyze how HEP compliance correlates with functional outcomes, visits, or patient satisfaction scores.
Driving Value Through Adherence to Home-Based Exercise
For growth-minded rehab organizations, boosting HEP compliance is a strategic imperative. By operationalizing these strategies to improve the HEP experience for your patients, organizations can improve outcomes, maximize therapist impact, reduce variability, and facilitate a more consistent journey.
With the right tools and systems in place, HEP adherence becomes more than a patient responsibility—it becomes an organizational strength.