Let’s be honest: Medicare is a good thing for lots of people who might not otherwise be able to access the healthcare they need. But Medicare billing? Well, it can be a headache, especially for the uninitiated. And with regular rule changes and a boom in Medicare patients on the horizon, it won’t get less complicated any time soon.
Here’s why:
Medicaid’s primary target population, adults over 65, is growing, and that age group is likely to need physical therapy more and more as they age. This demographic trend signals a big opportunity for your practice, but only if you get a handle on Medicare billing processes.
That’s exactly what this guide is all about. We’ll walk you through Medicare Part B billing basics to help you feel confident about securing more Medicare patients and revenue to grow your physical therapy practice.
Medicare Payments and Physical Therapy Billing 101
When it comes to Medicare billing, you first need to know the difference between Part A and Part B.
Medicare Part A covers inpatient services, including care delivered in hospitals and skilled nursing facilities. On the other hand, Part B focuses on outpatient care.
It’s also important to know that the Centers for Medicare and Medicaid Services (CMS) must deem physical therapy services necessary for a patient to receive care and for you to gain reimbursement.
1. Enrolling as a Medicare Provider
Ready to start accepting Medicare patients at your practice? You’ll want to sign on as a Medicare participating provider. That means you agree to accept Medicare’s fee schedule for covered services.
How to Enroll
The good news is the process of becoming a Medicare provider takes only three steps:
- Get your National Provider Identifier (NPI). An NPI is a unique identifying number for covered healthcare providers. You must use it in all your administrative and financial transactions with CMS. The quickest path to get an NPI is to apply through the National Plan & Provider Enumeration System (NPPES) website. Properly completed electronic applications can take fewer than ten days to process.
2. Complete your Medicare Enrollment Application. Next, you need to enroll as a Medicare provider through the Provider Enrollment, Chain, and Ownership System (PECOS). Be sure to check out the site’s videos to help you through the process.
3. Work with Your Medicare Administrative Contractor (MAC). Your MAC is a private health insurer that processes healthcare claims. MACs are the primary points of contact between Medicare programs and enrolled care providers.
Other Options
Being a Medicare participating provider is one path—and it’s the one most eligible medical providers take—but it’s not the only way.
Two alternatives are also available to you:
Non-participating provider. This choice means you’ll accept some Medicare patients but don’t always accept Medicare’s approved fees. If you elect to accept the assignment of a claim from Medicare, you’ll receive only 95% of the Medicare-approved rate. You can also bill patients more than the approved rate, but only up to 15% of the allowed amount.
Opt-out provider. If you go this route, you’ll need to sign an affidavit to opt out of the Medicare program completely. You can bill any amount you deem reasonable, and Medicare patients must sign an agreement stating they agree to be financially responsible for charges. This is a rare choice for rehab therapists, with just 1.3% opting out.
2. Submitting Medicare Claims: The Basics
If you’re going to submit a Medicare claim, you want to get it right the first time! That means less frustration and faster reimbursements, which is a clear win for your practice. Tackling denied claims is tricky, but we’ll give you tips to avoid that hassle.
Here are the basic steps involved in submitting Medicare claims:
Verify patient eligibility. As a first step, ensure the patient is enrolled in Medicare. Every beneficiary receives a card, including a unique identification number that you can use for online or phone verification.
Complete documentation. Medicare requires that all claims have supporting documentation to validate the necessity of provided services. Typically, this documentation includes the basics like date of service, reason for encounter, diagnosis, plan of care, and other essential details.
Submit an electronic claim. You can transmit electronic claims directly from your computer to your MAC to streamline processing. However, you must be using software that meets electronic filing requirements under the Health Insurance Portability and Accountability Act (HIPAA).
Track the status of your claim. After submission, each claim goes through two rounds of edits by your MAC. In a nutshell, edits are reviews of claims against HIPAA requirements. All claims are also subject to a 14-day waiting period before a payment decision. You can start checking on the status of your claim payment after this waiting period elapses.
Receive payment for approved claims. You’ll automatically receive electronic reimbursement for all approved Medicare claims.
- Appeal denied claims. You can appeal any Medicare coverage or payment decisions within 120 days after the notice that the claim was denied. There are multiple appeal levels, but your first step is to appeal to your Medicare Administrative Contractor.
What Systems Do PTs Use to Submit Medicare Claims?
Most physical therapists use electronic systems to submit Medicare claims. Yes, paper-based options are available, but they’re slower, less secure, and more error-prone.
One option is to send claims manually through your Medicare Administrative Contractor’s submission portal. You can look up your state’s MAC to ensure your routing claims to the right place.
But for an even faster, more seamless process, you can use specialized medical billing software that automates claim submission. Working with an outsourced medical billing service provider is another alternative.
While efficiency is always important, claim accuracy is a must—or else you’ll face a backlog of denials and slow reimbursements.
💯 Practical Advice
Want to keep denials low? Getting smart about preventing claims denials is your first order of business, but knowing how to navigate technical and clinical denials can make appeals less painful. Here’s another article on denial management tips.
3. Meeting CMS Documentation Requirements
CMS is a stickler for details, for good reason. After all, the agency is responsible for being a good steward of public funds. And that means avoiding waste, fraud, and abuse and ensuring that billed claims are for medically necessary services.
But it also means you need to be on top of your documentation game to meet CMS’s exacting standards. For example, you need to:
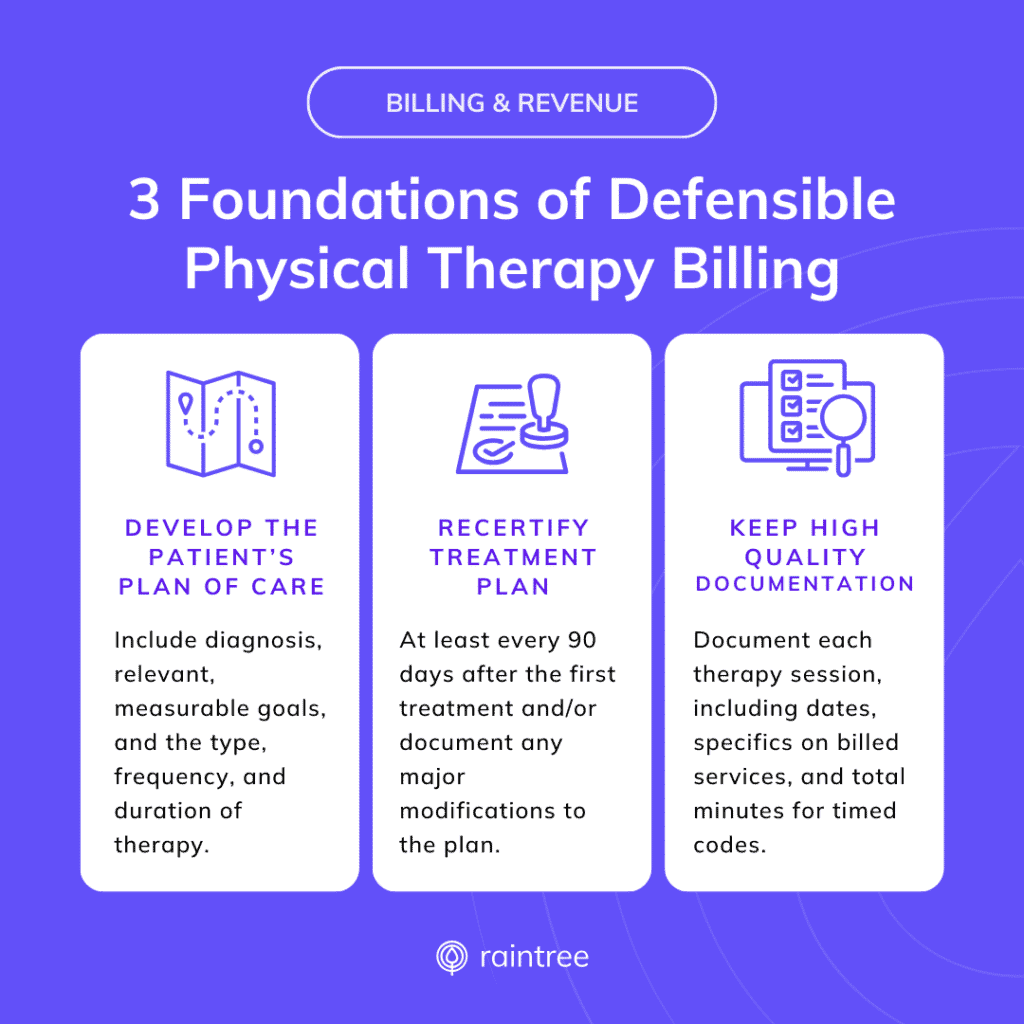
Develop specific treatment plans for each patient with a diagnosis, relevant, measurable goals, and the type, frequency, and duration of therapy.
Recertify treatment plans at least every 90 days after the first treatment and/or document any major modifications to the plan.
Keep thorough notes for each treatment day and service, including dates, specifics on billed services, and total minutes for timed codes and the full therapy session.
How to Prevent Medicare Claim Denials with Thorough Documentation
Accuracy matters! To prevent denials, you need to be on the lookout for these common errors:
Missing treatment plan certification and recertification. The approving physician, nurse practitioner, or therapist must sign every certification and recertification.
Incomplete signatures. Approving professionals must include a signature, date, and professional designation.
Incomplete plan of care (POCs). POCs should include full details on diagnoses, treatment types, frequency, and duration.
Lack of initial evaluation. Every patient must have an initial evaluation signed and dated by the approving professional.
Neglecting progress reports. Progress reports clarify medical necessity and support the frequency and duration of treatment.
Throughout the treatment journey, providers are responsible for verifying that there’s a reasonable expectation that patients can continue to make progress. If improvement is unlikely, CMS may not find it reasonable to pursue continued services or reimbursements.
4. Billing and Coding Best Practices for Medicare Reimbursement
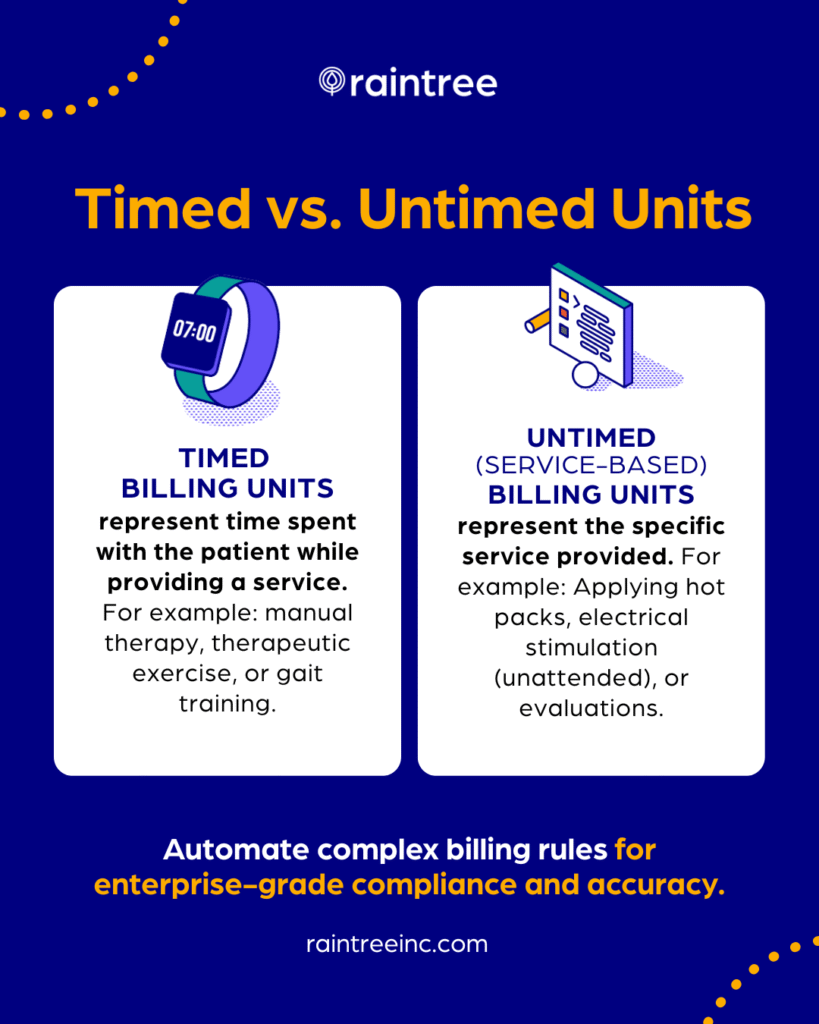
Physical therapy services utilize timed and untimed CPT codes. Timed codes represent 15-minute units of service provided, enabling accurate billing for total time spent on a patient’s therapy. By contrast, untimed codes, such as therapeutic procedures or manual therapy, are billed irrespective of the time expended.
But, as you undoubtedly know, care does not always fit neatly into 15-minute blocks. That’s why CMS instituted the 8-minute rule.
Simply put, whenever you spend more than eight minutes providing a service to patients, you can bill for the full 15 minutes.
To calculate how much to bill for timed care, add up the total time spent with your patient, then divide it by 15. Is your remainder more than eight? If the answer is yes, the 8-minute rule applies so you can bill for one more timed service unit.
Avoid Common Medicare Billing Errors
Medicare billing mistakes can unleash weeks of frustrating complications. From delayed or reduced payment to being at greater risk of a Medicare audit, each misstep takes its toll on your practice.
That’s why it’s wise to know and avoid common billing errors, such as:
Inaccurate CPT codes. All healthcare providers use standard billing codes, which may include Current Procedure Terminology (CPT) codes defined by the American Medical Association (AMA). With over 10,000 codes, it’s all too easy to apply the wrong one if you’re not careful.
Incorrect use of modifiers. You may need to add an extra two-digit code—called a modifier—to the end of a CPT or other billing code. These modifiers indicate that the service you provided was modified in some way, although not fundamentally changed. For example, there are specific modifiers that are only relevant for rehabilitation therapy. Applying a modifier for emergency services or surgery as a physical therapist would generate a denial.
Omission of necessary services on claims. CMS has specific rules about codes that can and cannot be billed together. For example, you can bill for therapeutic exercise or activity on the first day you see a new patient, but only if you bill for an evaluation as well. Just billing for the exercise or activity for a brand-new patient wouldn’t work, though.
5. Understanding Medicare Payments and Physical Therapy Reimbursement Rates
Your Medicare claim will undergo several processing steps and CMS checks to ensure it matches up to payable services before being approved for reimbursement. Once validated, CMS issues payment directly to your practice.
Several things influence the reimbursement rate, from codes and modifiers to your clinic location. The Medicare conversion factor (CF) also comes into play. While the conversion factor involves a complex calculation, the simplest explanation is that the CF is a scaling formula that adjusts the relative value units (RVU) of a specific medical service into a payment amount.
Another factor—the Medicare Incentive-based Payment System (MIPS)—influences your final payment amount. MIPS is part of Medicaid’s original Quality Payment Program (QPP), one pathway for eligible providers to collect and report performance data. Other programs for MIPS reporting include MIPS Value Pathways (MVPs) and Advanced Alternative Payment Models (APMs). Through MIPS, CMS seeks to reward providers who set a high bar for delivering quality care with payment boosts and reduces payments to those who don’t meet quality standards.
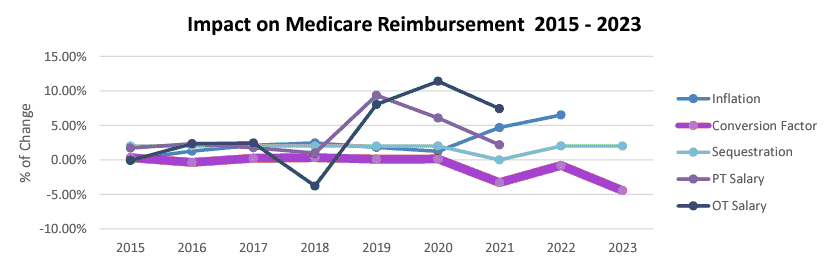
Source: National Association of Rehab Providers & Agencies (NARA)
6. Stay on Top of CMS Proposed and Final Rules
The good and bad news about Medicare billing standards is that they change regularly.
On a positive front, this can mean higher reimbursements and expanded service coverage. But the downside is that you must stay on top of changes, or else you put yourself at risk of costly, time-consuming denials.
The bottom line is that you need to keep up to date on CMS’s annual proposed and final rules. Each year, CMS issues a “proposed rule,” which essentially is a notification that it plans to issue or modify certain regulations. After a public comment period, CMS will develop and publish its final rule, with these rules taking effect 30 to 60 days after publication.
📢 Recently Announced
CMS released its Proposed 2025 Medicare Physician Fee Schedule in July, 2024. The proposal contained many updates (and some wins) relevant to physical therapy, as well as another dip in the conversion factor.
7. Compliance and Medicare Audits
The word “audit” spawns stomach-clenching discomfort for just about everyone. But when it comes to Medicare payments and physical therapy, one of the last things you ever want to face as is a CMS audit. Failing audits can lead to revocation of your Medicare billing privileges or fines of up to $1,000,000.
Medicare auditors look for signs of overbilling, improper coding, or billing for services that aren’t considered medically necessary. An error or two here and there won’t grab their attention, but repeated missteps are almost sure to send up a red flag.
To stay off CMS’s radar (and secure faster payments), you want to comply with Medicare billing standards. Following the tips we’ve covered here and using technology to reduce errors can keep you out of the audit danger zone.
More Efficient Medicare Reimbursement for Physical Therapy Services
While Medicare billing is unlikely to ever be easy, you can simplify the process with specialized technology.
Physical therapy software that helps your team generate accurate clinical documentation, streamlines claims submissions, and minimizes denied claims gives your revenues a big boost while lowering your administrative burden. Talk about a win-win!