There’s a lot to know when it comes to physical therapy reimbursement. Because payer guidelines in healthcare are highly regulated and prone to change, even minor mistakes can lead to denied claims.
That’s why we’re sharing these physical therapy billing examples: to help you get it right the first time, saving time, money, and headaches.
Evaluations and Re-Evaluations
First things first, let’s talk evaluations. The complexity of the patient’s case dictates the appropriate code—low, moderate, or high.
Low-complexity evaluations (97161): straightforward cases with minimal clinical decision-making
Moderate-complexity evaluations (97162): require more in-depth assessment and decision-making
High-complexity evaluations (97163): complex cases requiring comprehensive analysis and management
Re-evaluations (97164): assess progress or changes in a patient’s condition
Remember, accurate documentation is needed to justify the complexity level as well as ensure proper reimbursement. Utilize resources such as the American Physical Therapy Association (APTA)’s evaluation codes pocket guide. It includes nuances such as many payors no longer using the 97001 evaluation code and 97002 re-evaluation code, while claims for workers’ comp and auto liability may continue to use them.
Examples: Billing for Physical Therapy Evaluation
Evaluation of a new patient with post-surgical knee pain will likely warrant a “moderate complexity” evaluation code due to the surgery and the potential for multiple injuries or issues.
An existing patient with chronic low back pain, returning for a planned re-evaluation will likely use the same complexity level as the original assessment since re-evaluations don’t differentiate between complexities.
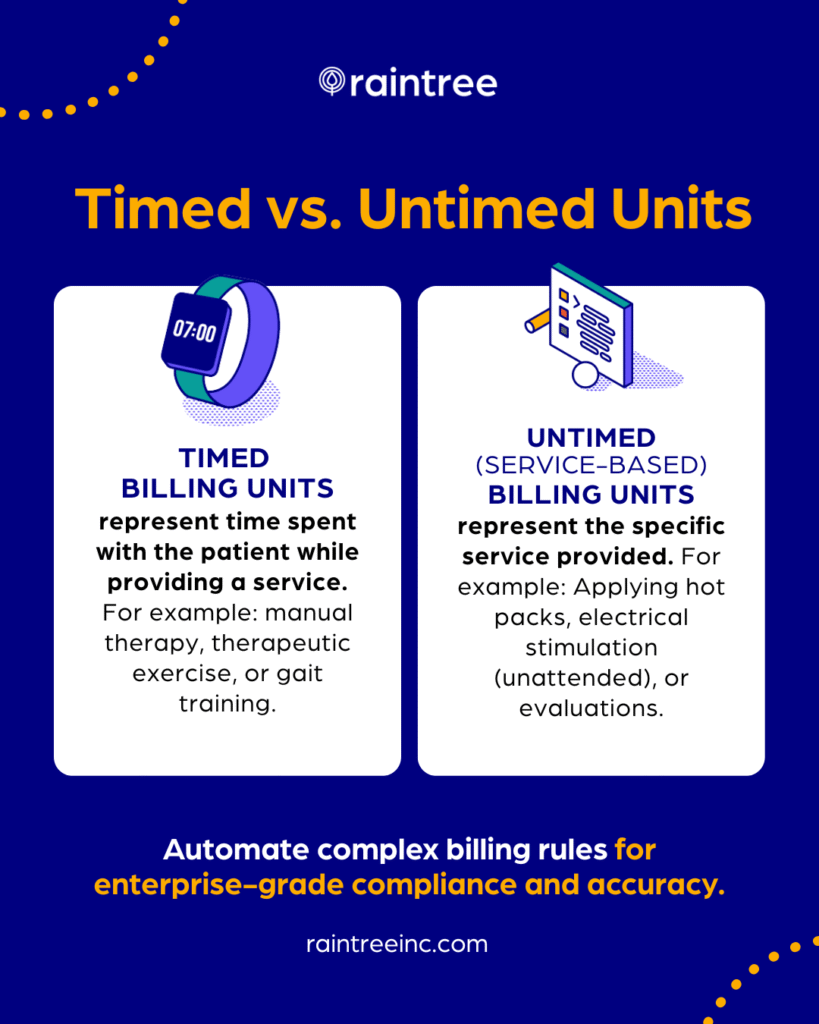
Physical Therapy Billing Units: Timed vs. Untimed Codes
Knowledge of timed and untimed codes is essential when billing for physical therapy services.
Timed codes, like 97110 (therapeutic exercise), are reimbursed based on 15-minute billing units for “hands-on” or therapist-guided exercises. Untimed codes, like 97535 (therapeutic activity), don’t require time-tracking but may have specific documentation requirements.
Medicare Billing and Mixed Remainders
Can you get reimbursed when the total time spent providing multiple timed services doesn’t fall perfectly into 15-minute increments? For Medicare Part B patients, CMS allows billing for these “remainders” as long as the sum is at least 8 minutes.
Always document the total time spent on each service as well as the rationale behind your chosen billable units. Clear, detailed records help avoid denials.
Example: Applying Mixed Remainders
You provide 18 minutes of manual therapy (97140) as well as 9 minutes of gait training (97116). Individually, neither surpasses the 8-minute rule threshold. However, combined, their total (27 minutes) exceeds it (27-15=12). So, bill for one additional unit of manual therapy since it represents the higher portion of time (3 vs. 1).
💯 Practical Advice
Not all payers adhere to the Medicare 8-minute rule, nor do they necessarily allow billing for remaining minutes in the same way.
Group Therapy vs. Concurrent Therapy Services
Differentiating group therapy from concurrent therapy can be tricky. While both involve multiple patients receiving treatment, they differ in terms of provider involvement and reimbursement.
The key difference has to do with your patients’ treatment goals. Group therapy targets similar goals, while concurrent therapy addresses individual needs.
And it’s important to keep in mind: Group therapy requires documenting each patient’s participation, while concurrent therapy should include detailed records of each patient’s treatment plan and progress.
Examples: Billing for Group Therapy vs. Concurrent Therapy
Group Therapy. Three patients with similar conditions participate in a 30-minute group treatment session focused on strengthening exercises. Treatment is billed as 1 unit (15 minutes) per patient (2 units total).
Concurrent Therapy. Treating two patients simultaneously, each with different diagnoses and treatment plans. Each patient receives 30 minutes of treatment. This billing scenario requires separate claims for each patient based on their specific interventions (e.g., 2 units of therapeutic exercise for one and 2 units of gait training for the other).
Co-Treating as a Physical Therapist
Co-treating is when two therapists from different disciplines treat a patient in the same session. Both therapists contribute specialized expertise to establish a clear plan of care for the patient, and share progress updates and modifications as needed. This approach can lead to improved patient outcomes.
Payer guidelines dictate how co-treating sessions can be billed, and may vary depending on the specific therapy disciplines involved.
Examples: Co-Treatment
A patient requires physical and occupational therapy to treat a post-surgical shoulder injury. The physical therapist (PT) works on improving range of motion and strength, while the occupational therapist (OT) focuses on the patient’s functional abilities like dressing or self-care. Each can bill for the entire session as long as documentation justifies the necessity of co-treatment and outlines each therapist’s distinct contributions.
- A physical therapist and speech-language pathologist (SLP) co-treat a patient with swallowing difficulties. The PT focuses on oral motor exercises, while the SLP addresses communication strategies plus cognitive aspects. Only one therapist can bill for the entire session. Other options include both therapists billing for half of the session, but the 8 minute rule still applies!
CCI Edits
CCI (Correct Coding Initiative) edits stipulate which codes can’t be billed together.
By applying CCI edits, physical therapy practices can avoid billing errors, denials, and potential audits. Regularly review code descriptions and payor guidelines to understand which code takes precedence in case of conflicts.
Examples: CCI Edits in Physical Therapy Billing
You co-treat with an OT. Both of you bill for therapeutic exercise (97110). This duplicate billing for the same service raises a red flag. Only one therapist can bill for the exercise intervention, with the other potentially utilizing untimed codes for distinct contributions like patient education or activity assistance.
You bill 97140 (manual therapy) and 97124 (massage therapy) for the same session. This triggers a CCI edit because these are mutually exclusive procedures and can’t be billed together, even with a modifier. In other words, you can treat a patient’s injury with one of these types of therapies in a session, but not both.
Don’t Forget Your Modifiers
Many codes can be billed together if a modifier is added.
Adding a modifier 59, for example, clarifies that both services were provided separately. Any two time-based services should be performed within their own 15-minute increment(s), not both within the same time frame.
Per APTA, The X modifiers (XE, XS, XP, XU) should be used in place of modifier 59 if one of them more specifically describes the reason both codes should be paid.
Thorough documentation should be included justifying your chosen code or if there’s any doubt about two codes being billed together for the same patient during the same session.
CPT Code 97799
CPT code 97799, often dubbed the “miscellaneous charge code,” serves as a catch-all for procedures not covered by standard codes.
While it provides flexibility for unique or experimental treatments, its misuse can lead to billing discrepancies and potential audits. Physical therapy practices must use it judiciously and always explore alternative, specific codes before resorting to CPT 97799.
To use this code correctly, it may be necessary to confirm insurance coverage or obtain pre-authorization for certain services.
Example: Using CPT 97799
- A patient is treated with a non-traditional PT intervention such as acupressure or therapeutic horseback riding. You bill code 97799. This raises red flags for insurers, as the code lacks specific treatment details. Documentation justifying its use and alignment with the therapy plan of care becomes crucial to avoid denials.
💯 Practical Advice
Use code 97799 sparingly—only for unlisted services supported by strong clinical rationale, documentation, and adherence to payor guidelines.
Out-of-Network Billing Scenarios
Out-of-network billing in physical therapy requires careful consideration and documentation to maximize reimbursements while maintaining compliance. Unlike in-network billing, where rates are negotiated with insurance companies, out-of-network billing allows providers to set their own rates.
However, patients may be responsible for a larger portion of the costs, as out-of-network services often have higher out-of-pocket expenses.
When billing for out-of-network, ensure proactive and transparent communication with patients regarding potential costs and coverage limitations.
Examples: Out of Network Billing for Physical Therapy
Your practice specializes in vestibular rehabilitation, a niche service not readily available in-network. A patient seeks your expertise and is willing to pay out-of-pocket. Communicate your out-of-network status early on, provide transparent cost estimates, and explain the potential benefits of specialized care.
A patient’s in-network provider isn’t accepting new patients, but their insurance plan allows out-of-network coverage. You agree to treat them and verify their out-of-network benefits, including deductibles, coinsurance, and any limitations. Offer flexible payment options and consider filing claims on their behalf to maximize their potential for reimbursement.
Examples of Billing Mistakes That Will Cost You
Knowing what to look for as well as implementing preventive measures can help you avoid mistakes, build trust with payors, and deliver exceptional patient care.
Common Billing Errors
❌ Billing a code (e.g., 97110 for therapeutic exercise) as one unit for 25 minutes, forgetting the 8-minute rule. This could lead to a denial.
✔️ Double-check coding guidelines and familiarize yourself with time-based rules.
❌ Your notes lack specific details about the interventions provided during a session. This inconsistency between documented services and billed codes raises red flags for insurers and increases risk of lost revenue.
✔️ Maintain meticulous documentation that accurately reflects each treatment you provide.
❌ You neglect to verify a patient’s insurance eligibility and benefits before providing treatment, causing unexpected costs for the patient or your clinic if the claim gets denied.
✔️ Always verify insurance information upfront and monitor coverage changes.
❌ You submit claims past the deadline set by the payer. Late submissions often result in automatic denials, jeopardizing your reimbursement.
✔️ Develop a system for timely claim submission to avoid missing deadlines.
Securing Reimbursement: Billing Software for Physical Therapy
So, as you can see, there’s a lot involved in physical therapy billing. Billers must be knowledgeable and stay up to date with changes.
Specialized PT billing software can help automate tasks like coding, claims, and payments, preventing errors through built-in checks and templates. Efficient systems also support quality clinical documentation and compliance with real-time verification and guidance.