Medical billing and coding compliance requires healthcare organizations to accurately document services for reimbursement, while adhering to federal regulation and private payers’ requirements.
Easier said than done! Keeping up with ethical coding standards and billing best practices is complicated.
To break it down for you, Raintree Systems’ Chief Compliance Officer, Veda Collmer, JD, CIPP/US, joined the Therapy Matters podcast to talk about medical billing compliance. The conversation centered on three major topics: fraudulent claims, adherence to HIPAA regulations, and the utilization of certified electronic health record technology (CEHRT).
1. Fraudulent Claims and Billing Compliance Issues
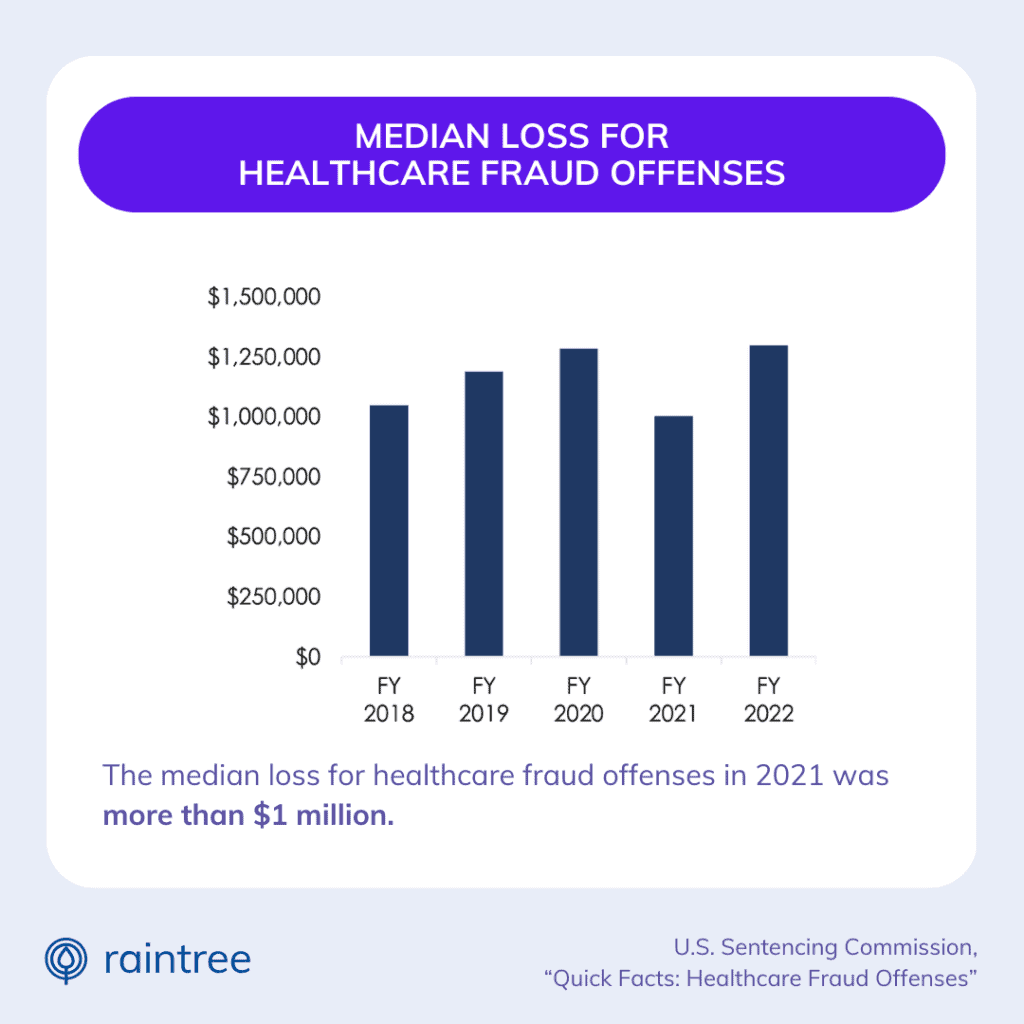
Fraudulent healthcare billing is a major problem in the U.S.
Common forms of medical billing fraud include upcoding, unbundling (also known as “fragmentation”), double billing, or phantom billing. In each of these cases, fraud occurs when a healthcare organization bills government or private insurance providers for services they did not provide.
Let’s dig into that. Upcoding, for example, refers to deliberate billing of services at higher levels of complexity than the actual medical services provided or documented. This definition comes from a publication of Health Economics Review, which also reported that, on average, “upcoding for physician services under Part B is $2.38 billion annually (or 2.43% of Part B annual expenditures).”
Breaking medical coding and billing rules and regulations can result in hefty fines—and even prison time. And while intent does play a role in unethical billing practices—when the provider knowingly and willingly commits fraud—clinics can get in trouble simply for being sloppy with their billing, or making honest mistakes.
Preventing Coding and Billing Errors
Collmer says that the first step to preventing billing errors is to recognize that compliance is complicated, and managing the billing process is highly skilled work. You need the right tools and internal resources to tackle this piece of the revenue cycle accurately and efficiently.
For some practices, that may mean adopting a system that streamlines claims and billing workflows. This could include automated alerts or built-in coding guidelines that reduce billing and coding errors. Some practices may also enlist the help of third-party billing companies or revenue cycle management solutions.
“I don’t change my own oil, I don’t do my own taxes—I hire professionals,” says Collmer. “The same goes for billing.”
2. HIPAA Regulations and Patients' Right of Access
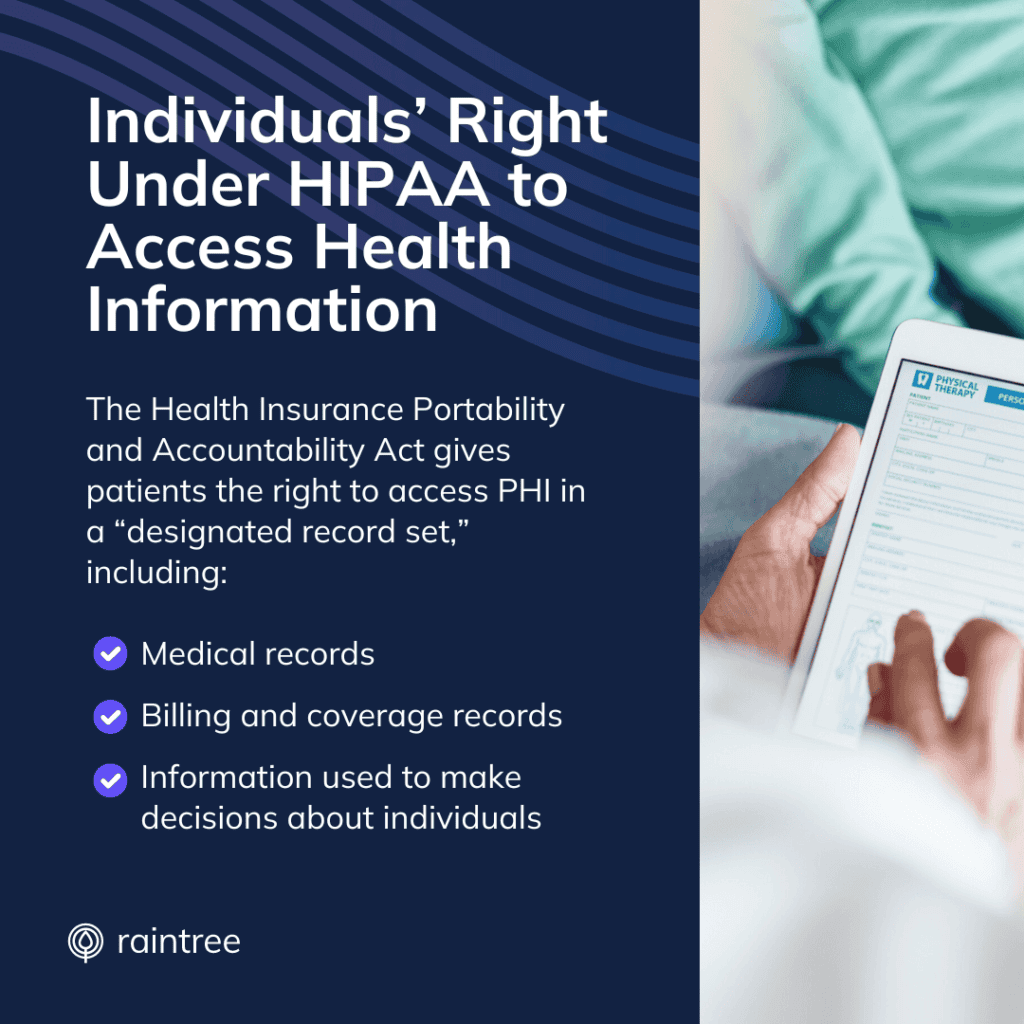
If you’re part of the healthcare industry, you must be familiar with Health Insurance Portability and Accountability Act (HIPAA). HIPAA regulations are enforced by the Department of Health and Human Services, and are designed to protect patients’ sensitive information.
Enforcement trends change over time, but Collmer says that one area in particular is taking center stage: patients’ right to access their medical records.
Ensuring Patients' Right to Access Medical Records
Under HIPAA, clinics and practices are required to grant patients timely access to their own medical records. Practices also cannot charge exorbitant fees to patients when providing their own records to them.
Ensuring compliance in this area is important, Collmer says. “Patients know that they have this right, and they’ll easily make a complaint.” Practices that knowingly and willingly restrict patient access to their own records can face steep penalties of up to $1.5 million.
One of the best ways to stay compliant and provide patients with the most up-to-date information is to offer a modern patient portal that’s integrated with your electronic health record (EHR) system.
3. Utilizing Certified Electronic Health Record Technology
To understand the importance of certified EHR technology for your practice’s revenue, let’s look at the bigger picture of the healthcare and regulatory landscape.
As of now, most healthcare practices and organizations in the U.S. have transitioned away from paper-based recordkeeping. This process required the adoption of electronic medical record (EMR) or electronic health record (EHR) systems. At the start, EHR systems were primarily designed for the needs of hospital systems, while EMRs were the preference of outpatient practices and specialists.
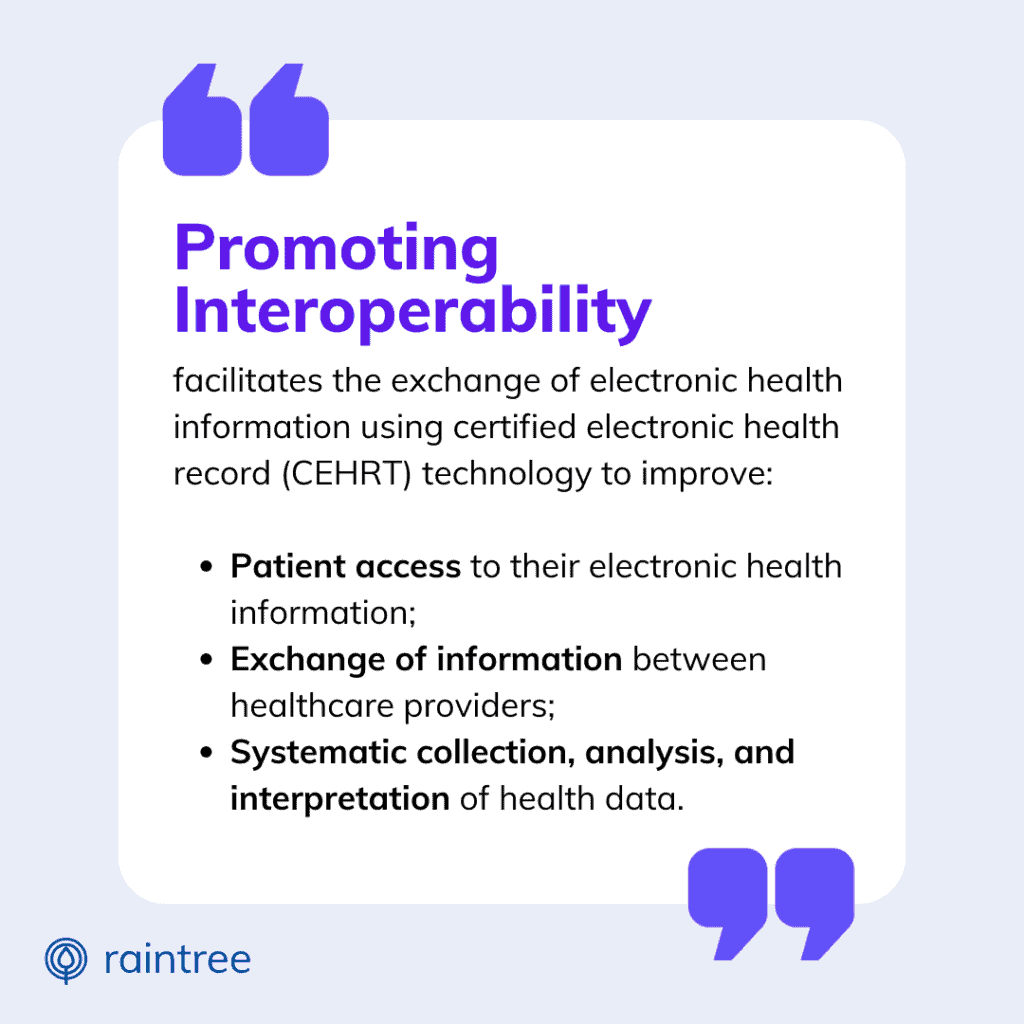
Though the terms are often used interchangeably, and they provide the same basic functionality (storage and management of electronic PHI) there are certain differences between EMR and EHR software. Notably, EHR software typically refers to systems that have earned Office of National Coordinator (ONC) certification.
“To be able to achieve that certification standard through the ONC is a high standard,” Collmer said. The process requires third-party verification of certain functionality, proving its capability of supporting care coordination and interoperability.
Using Certified EHR Can Affect Future Medicare Payments
With the gradual movement toward value-based care and health data sharing, physicians and specialists have been incentivized by federal payment programs to adopt EHR technology. For example, updates to the most recent Medicare Physician Fees Schedule have solidified the connection between adoption of certified EHR technology and MIPS payment adjustments.
“I think it helps us to think [that] these aren’t just compliance boxes we’re checking. There is a bigger vision here,” Collmer says.
To learn more about Medicare billing compliance and MIPS reporting, visit our MIPS resource center.
Managing Medical Billing Compliance
Are you feeling overwhelmed by the balancing-act of medical billing compliance? It’s time to take decisive control over your revenue cycle. Using the right technology, rehab therapy organizations can streamline your manual billing processes and minimize the risk of billing errors.
With real-time status alerts, billing workflows, reports and dashboards, Raintree helps practices ensure that clinical documentation and claims adhere to the latest payer and state codes. Additionally, Raintree leads the industry on compliance and is currently the only ONC-certified EHR system designed for PT, OT, and SLP.

Allison Jones was Vice President of Marketing at Raintree Systems. In her role, she was responsible for defining, shaping, and leading the company’s strategic marketing direction. Before joining Raintree, she was Vice President of Marketing at eMDs, a CompuGroup Medical company. She has also held various marketing roles in the printing, publishing, and infosec industries.
Frequently Asked Questions
What is medical billing and coding compliance?
Medical billing and coding compliance refers to adhering to the rules and regulations set by governmental and private payers in order to ensure accurate and ethical billing practices within the healthcare industry.
Why is billing compliance important for medical practices?
Billing compliance is crucial for medical practices to avoid legal issues, audits, and financial penalties. It also ensures accurate reimbursement for services rendered.
What are the consequences of non-compliance in medical billing and coding?
Non-compliance in medical billing and coding can lead to legal repercussions, financial penalties, reputational damage, and exclusion from participation in federal healthcare programs.
How can healthcare providers ensure compliance in medical billing?
Healthcare providers can ensure compliance in medical billing by implementing a robust compliance program and staying up-to-date with the latest regulatory requirements. Best practices for coding compliance include maintaining accurate medical record documentation, ensuring coding accuracy, and following established coding guidelines.
How can medical practices design an effective healthcare compliance program?
Medical practices can design an effective healthcare compliance program by establishing a culture of security and compliance, providing training to staff, conducting regular risk assessments, and addressing compliance issues promptly.